본 연구는 구강건강상태와 감지 건강상태의 연관성을 조사하기 위하여 구강건강상태지표인 우식경험영구치지수와 지역사회치주지수를 조사하였고 감지 건강상태를 조사하기 위하여 건강과 관련한 삶의 질을 평가하는 지표인 EQ-5D를 조사하여 위 변수들의 연관성을 조사분석하여 다음과 같은 결론을 얻었다.
전신 움직임에 문제가 있다고 응답한 대상자들의 우식경험영구치지수가 1.18배 높았으며 동통 및 불편감에 문제가 있다고 응답한 대상자들의 우식경험영구지지수가 1.16배 높았고 감지 건강상태와 치주병은 연관성이 없었다.
결론적으로, 감지 건강상태는 우식경험영구치지수와 유의한 연관성이 관찰되었다. 따라서 감지 건강상태(EQ-5D)는 구강건강상태를 예측하는 지표로 추천할 수 있으며 나아가 삶의 질을 증진시키는 객관적인 도구로도 활용 가능하다고 생각된다.
Single-item global self-rating symptoms are frequently used to measure health status1). They have been reported to perform well in predicting mortality and morbidity, screening for high-risk groups2). Such global self-ratings have been used to assess general health, and also to asses oral health status3,4). Health is a state of complete physical, mental and social well-being not merely the absence of disease or infirmity5). By such a definition, it is implied that one’s perception of general health can practically be associated with one’s state of oral health. A Patient’s self-rating oral health often does not correspond to a practitioner’s evaluation6). Many researchers have investigated association between perceived general health and perceived oral health3,4). Locker et al.3) suggested that older adults’ rating of oral health are associated their rating of general health. At the same time, many studies7-9) have been reported to be associated between objective oral health status and perceived oral health.
Some researches10-12) investigated the association between oral inflammation and general health disease such as stroke, cardiac disease, diabetes, and so on. This association can influence self-rating general symptom in those who have oral disease associated with general health problem.
As a matter of fact, objective findings of oral health status cannot simply be converted into subjective perceptions of general health conditions as not only pain and loss of function derived from oral diseases but also socioeconomic factors such as gender, race, level of education, and oral health related behaviors. So, it needs to declare the relationship in a model reflecting clinical factors, demographic and socioeconomic factors and oral health related behaviors. Moreover, it was reported that quality of life was improved after dental rehabilitation13). However, an effort to analyze the association with general health perceptions in such comprehensive models was rare14,15).
The EuroQol items can be used as a descriptive system to illustrate health problem, or they can be used in conjunction with value sets and algorithms to estimate health state utility values16). For this analysis the EuroQol-5D (EQ-5D) used as a descriptive system, with the presence of a health problem defined as either ‘some’ or ‘extreme’, and classified into the two strata of 1 non-health problem and 2∼3 health problem.
Increase of chronic disease has suggested the need of the index which included not only complex disease status but also patient’s perceived health symptom17). Recently EQ-5D was a tool as health-related life quality in the world.
Decayed, missing, and filled teeth (DMFT) index or community periodontal index (CPI) has been utilized in order to establish or evaluate new policies concerning oral health in Korea. It is crucial to understand the virtue of self-rating general health when formulating oral health policies that can substantially help elevate status of health and therefore the quality of life. This study aims to analyze such relationships between perceived general health and oral health status.
We analyzed 14,231 subjects aged 30 years or older who participated in Korea National Health and Nutrition Examination Survey (KNHANES; 2007∼2009). Subjects aged between 30 and 89 years, and included 42.3% male and 57.7% female. Non-respondents on health variables were excluded.
All individuals were examined by a questionnaire about socioeconomic history, smoking and drinking habit, the frequency of daily tooth brushing and the presence of regular dental visit. Dental survey was conducted to find the DMFT index and CPI.
Objective determinants of oral health status were recorded by DMFT and CPI code while demographic factors were determined by a self-recording questionnaire inclusive of age, gender, income level, education level, and oral health-related behavior such as the presence of regular dental check up and frequency of tooth brushing.
The EuroQol was used to evaluate general health of subjects16). The EuroQol contains health status descriptive system (EQ-5D), and records the level of self-reported problem according to five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). Each of the dimensions is assessed based on a single question with three response levels (no problem, some problem, and extreme problems).
Dichotomous variables are presented as percentages variables of oral health status of subjects with chi-square test. Multivariate logistic regression analyses were used to analyze the association of the perceived general health parameter with oral health variables. All variables were entered into the multivariate model with adjustment for age, gender, income, education, regular dental visit, tooth brushing frequency, smoking, drinking, and odds ratios and 95% confidence intervals are given for all factors. All statistical analyses were conducted using with SPSS 15.0 (SPSS Inc., Chicago, IL, USA).
1. DMFT index and socioeconomic status
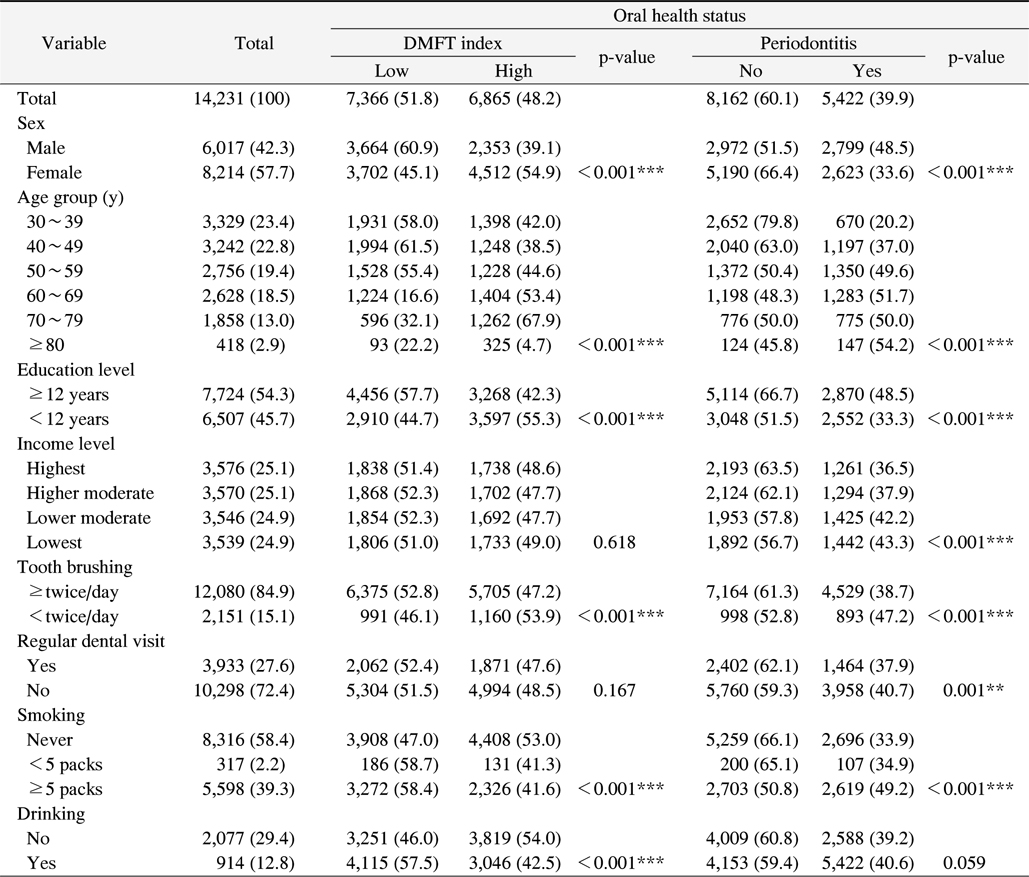
Male participants responded 42.3% of the participants was male, who responded relatively better perceived general health than female group (p<0.01), 48.2% of the participants had high DMFT index (≥7), and 39.9% of the participants had periodontitis (CPI≥3). DMFT index and CPI became higher as age increased (p<0.01). Oral health became better as education level increased (p< 0.001).
Of subjects, 84.9% participants brush the teeth over twice per day, and 27.6% of the participants have visited dental clinic for regular check-up. Periodontal health became better as tooth brushing frequency and regular dental visit increased (Table 1; p<0.001). Periodontal health became better as smoking decreased (Table 1; p< 0.001).
[Table 1.] Sociodemographic Characteristics of Subjects according to Oral Health Status
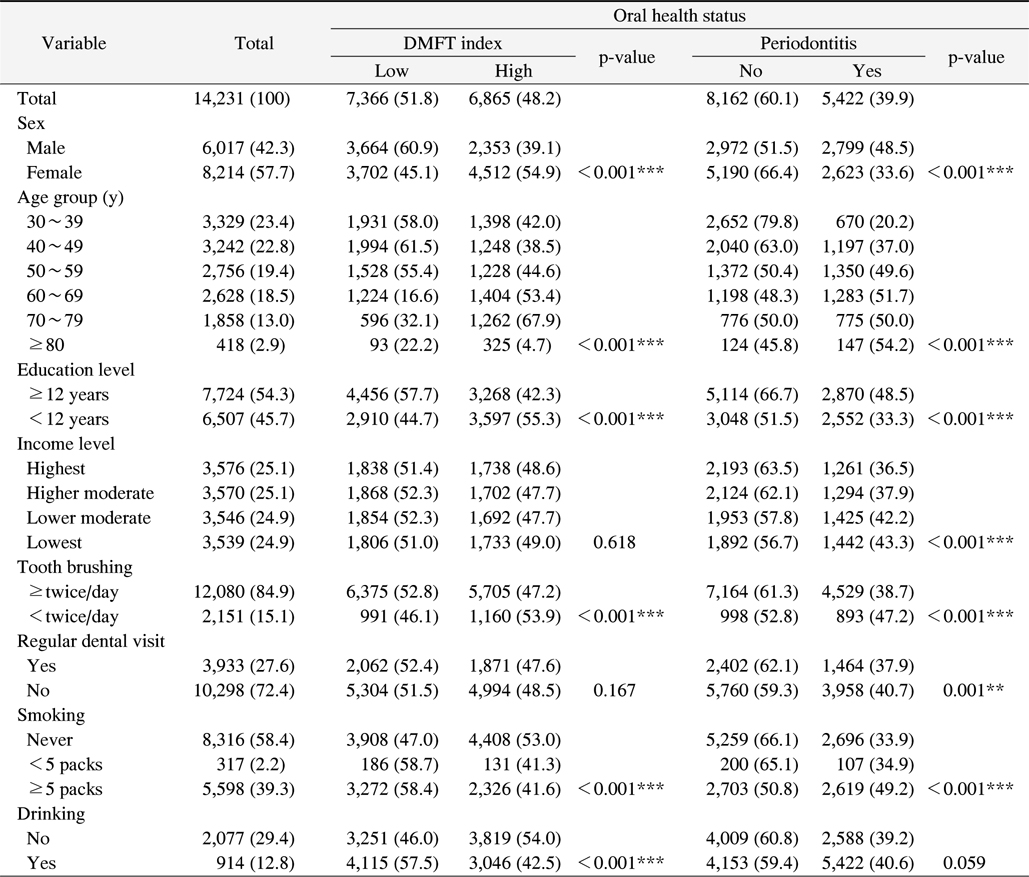
Sociodemographic Characteristics of Subjects according to Oral Health Status
2. Perceived general health symptoms and oral health variables
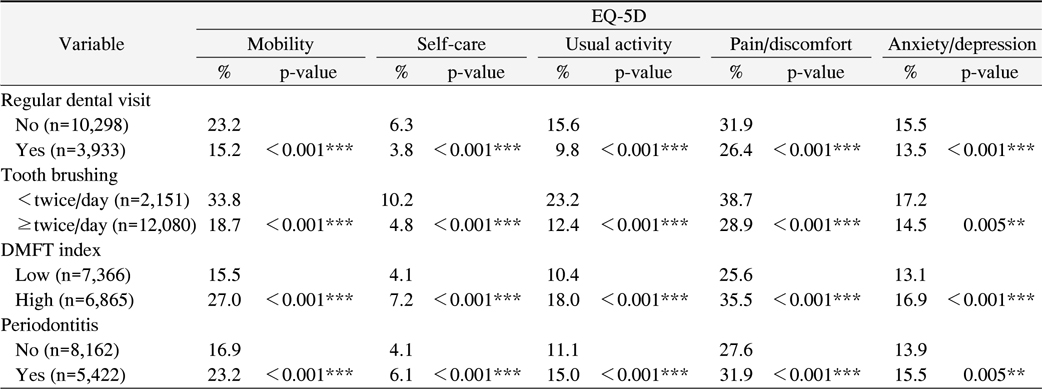
The group with regular dental visit had better self-rating general health symptom (p<0.001). The group with more tooth brushing frequency had better self-rating general health symptom (p<0.01). The group with high DMFT index had relatively worse self-rating general health symptom (p<0.001). Table 2 showed that 27% of those with higher DMFT index had problem with mobility, 7.2% with self-care, 18.0% with usual activity, 35.5% with pain/discomfort, 16.9% with anxiety/depression. For subjects with lower DMFT index, the percentages were 15.5%, 4.1%, 10.4%, 25.6% and 13.1%, respectively.
[Table 2.] Oral Health Variables of Subjects according to EuroQol-5D (EQ-5D)
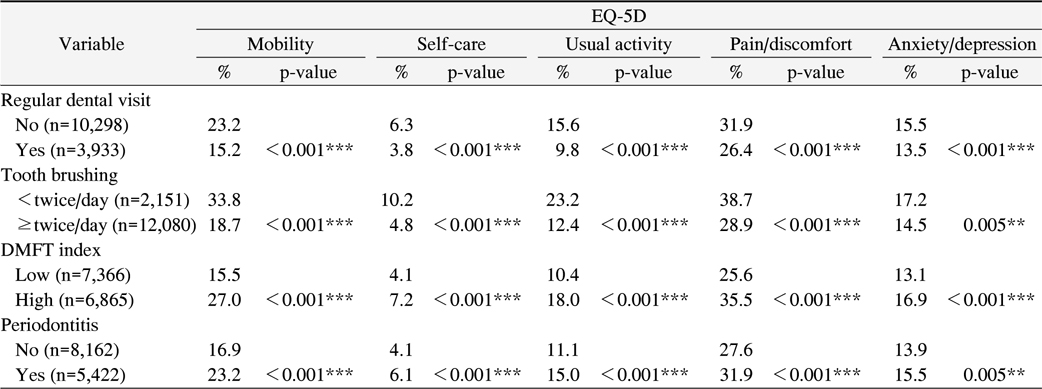
Oral Health Variables of Subjects according to EuroQol-5D (EQ-5D)
And 23.2% of those with periodontitis had problem with mobility, 6.1% with self-care, 15.0% with usual activity, 31.9% with pain/discomfort, 15.5% with anxiety/depression. For subjects without periodontits, the percentages were 16.9%, 4.1%, 11.1%, 27.6% and 13.9%, respectively. The group with periodontitis had relatively worse self-rating general health symptom (Table 2; p< 0.001).
3. Perceived general health symptoms and oral health status (in multivariate analysis)
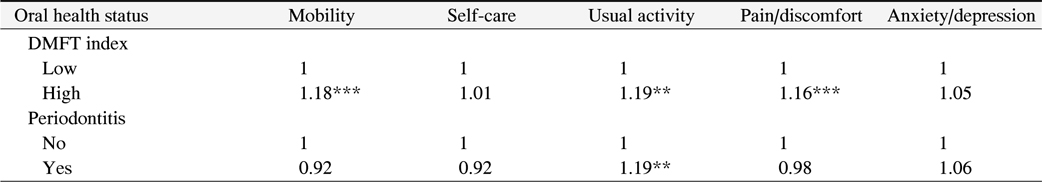
In a multivariate analysis adjusted for socioeconomic status, smoking, drinking, tooth brushing frequency, regular dental visit, the odds ratio of high DMFT index increased by 1.18 time in the subjects with perceived problem of mobility. The odds ratio of high DMFT index increased by 1.16 time in the subjects with perceived problem of pain/discomfort. However, periodontitis was not associated with EQ-5D (Table 3).
[Table 3.] Adjusted Odds Ratio of Oral Health Status for Perceived General Health Symptons
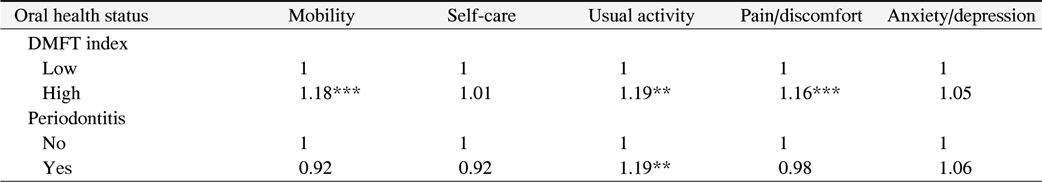
Adjusted Odds Ratio of Oral Health Status for Perceived General Health Symptons
This study investigated to find relationships between perceived general health symptom and objective oral health status in Korean adults, and showed that self-rating general health was positively associated with oral health, in particular with DMFT index.
Locker18) established a model in which self-rating oral health status was found to be associated with oral symptoms and functional limitations. It was said that such oral pain and discomfort would affect mastication that eventually would influence self-rating oral health status. Improved oral health was reported to be associated with improved self-rating general health13).
It was also found that perceived general health symptom was significantly related DMFT index (Table 2). Generally, DMFT index was reported with be related with gender, age, socioeconomic status, oral health behavior, smoking and drinking19,20). DMFT index was higher in female group than in male group in this study as other results19,20). This tendency was consistent with other reports19,20). Also, periodontitis had a tendency consistent with DMFT index. DMFT index and periodontitis become worse according to ages. Moreover, periodontitis was more prevalent in male group than female group. And, regular dental visit and tooth brushing frequency were associated with EQ-5D (Table 2). This result can be demonstrated that good oral health behavior can influence satisfaction of general health21), also can effect on objective oral health, so good oral health behavior can be associated with EQ-5D. Furthermore, DMFT index and periodontitis were associated with EQ-5D (p<0.001). Problem with pain/discomfort was most prevalent among 5 dimensions to be compared with oral disease. Subjects with problem of pain/discomfort were 35.5% in the subjects with high DMFT index and 31.9% in the subjects with periodontitis. Actually, other problem with EQ-5D was ranged from 6.1% to 27.0%. This result can demonstrate that subjects are sensitive to pain/discomfort. Moreover, DMFT index was associated with perceived problem of mobility and perceived problem of pain (discomfort) in multivariate analysis with adjusted with socioeconomic status, smoking, drinking, tooth brushing frequency, and regular dental visit (Table 3; p<0.001). The odds ratio of self-rating perceived problem with mobility and pain (discomfort) increased between 1.16 time and 1.18 time with increasing DMFT index. In concerning about relationship DMFT index and problem with mobility, problem with mobility was not thought to be associated with dental caries prevalence, but we can consider that questionnaires about health-related quality of life are related with one another. This relationship can demonstrate that specific disease unconnected with mobility such as dental caries can be associated with problem with mobility.
On the other hand, periodontitis was not associated with EQ-5D. It can be understood that DMFT can make so much pain than periodontal disease. Thus, the number of DMFT was thought to be associated with EQ-5D. Additional study is necessary to investigate the association between periodontal disease and health-related quality of life.
Generally, Korea has been utilizing only standard indicators such as DMFT index and CPI to establish or evaluate oral health policies so far. The above mentioned perceived general health symptoms are not only easy to assess but also flexible in reflecting objective oral health status, socioeconomic status and psychological influences. Therefore, the self-rating system of perceived health symptoms can be implemented in addition to the objective indicators to improve oral health care and enrich the qualities of life in advance. Health-related quality of life is typically measured using disease-specific measure in general, however it may be used together in order to address both clinical and broader policy question.
The strength of our study was that these data were obtained from a nationwide population with a high response and therefore provided representative information on the Korean population. Nevertheless, several study limitation should be considered. First, we did not assess all of life quality-related disease such as cardiovascular disease, body mass index and so on. Second, we can not infer causal relationship between oral health status and ED-5D in this cross-sectional study. Third, we could not measure health related quality of life using an oral health-specific quality of life tool, and only ED-5Q was measured in KNHANES. So, further studies are needed that disease-specific quality of life tools to assess the association between oral health and self-rating general health.
This study aims to analyze the association between perceived general health symptom and oral health status and has investigated oral health such as DMFT index and periodontitis and perceived general health symptom such as EQ-5D. The following conclusion was drawn. Subjects with perceived problem with mobility and pain/comfort had higher DMFT index (p<0.001). In conclusion, perceived general health was associated with DMFT index. It is recommendable that we can use the perceived general health to predict oral health. The self-rating system of perceived general health symptoms can be implemented in addition to the objective indicators to improve oral health care and enrich the qualities of life in advance.