Bee venom pharmacopuncture (BVP) is a new type of treatment combining the efficacy of acupuncture and the pharmacological actions of bee venom. The venom from live honey bees (
Sweet Bee Venom (SBV) was developed to circumvent these problems with BVP [9, 10]. SBV has more clinical uses than BVP, due to absence of the allergen in the original BVP that causes hypersensitive reactions. Previous studies showed that SBV was associated with fewer allergic responses than was BVP [11, 12].
In previous toxicology studies, Kwon
To provide comparative data, we evaluated the toxicity of SBV in a 13 weeks, repeated dose test on Sprague-Dawley (SD) rats and ascertained the No Observed Adverse Effect Level (NOAEL) dosage for SBV. This study was conducted according to guidelines established by the Organization for Economic Cooperation and Development (OECD) for the testing of chemicals in accordance with modern Good Laboratory Practice Regulations.
Fifty-five SD rats of each gender were obtained from a specific pathogen-free facility (Biotoxtech, OhChang, Korea) at 5 weeks of age and were used after a week of quarantine and acclimatization. The animals were housed in a room maintained at 20 ± 3℃ under a relative humidity of 52 ± 10%. The room was illuminated with artificial lighting from 07:00 to 19:00 and had a 10 to 15 minutes air change every hour. The animals were housed in suspended stainless- steel wire-mesh cages and were allowed sterilized tap water and commercial rodent chow (Teklad Certified Irradiated Global 10% Protein Rodent Diet 2918C). This study was performed in compliance with the test guidelines from the Korea Food and Drug Administration (KFDA) under the Good Laboratory Practice Regulations for Nonclinical Laboratory Studies. The study protocol was approved by the institutional Animal Care and Use Committee according to the “Guidelines for Toxicity Tests of Drugs and Related Materials, Document #2005-60” as prepared by KFDA (2005). Fifty-five SD rats of each gender were obtained from a specific pathogen-free facility (Biotoxtech, OhChang, Korea) at 5 weeks of age and were used after a week of quarantine and acclimatization. The animals were housed in a room maintained at 20 ± 3℃ under a relative humidity of 52 ± 10%. The room was illuminated with artificial lighting from 07:00 to 19:00 and had a 10 to 15 minutes air change every hour. The animals were housed in suspended stainless-steel wire-mesh cages and were allowed sterilized tap water and commercial rodent chow (Teklad Certified Irradiated Global 10% Protein Rodent Diet 2918C). This study was performed in compliance with the test guidelines from the KFDA under the Good Laboratory Practice Regulations for Nonclinical Laboratory Studies. The study protocol was approved by the institutional Animal Care and Use Committee according to the “Guidelines for Toxicity Tests of Drugs and Related Materials, Document #2005-60” as prepared by KFDA (2005).
The SBV was prepared using a freeze dryer (FD 8508, Ilshin Lab Co., Ltd., Namyangju, Korea) by G&V Co. (Wonju, Korea) and stored at —20℃. A high-performance liquid chromatography (HPLC, Agilent 1100 series, Agilent Technologies Ltd., Santa Clara, CA, USA) analysis was performed to confirm that the SBV was pure melittin.
Fifty healthy male and 50 healthy female rats were selected by average weight and assigned to 1 of 4 groups: control (normal saline, 0.2 mL/kg), low-dosage (0.07 mg/kg, 0.2 mL/kg), medium-dosage (0.14 mg/kg, 0.2 mL/kg), and high-dosage (0.28 mg/kg, 0.2 mL/kg) groups. The control and the high-dosage groups consisted of each gender 15 rats, 30 total rats in each of two groups, while the low- and the medium-dosage groups consisted of 10 rats of each gender, 20 total rats of the two groups. SBV was administered to the rats by intramuscular injection in both thigh muscles at a dose of 0.2 mL/kg once per day for 13 weeks. The control group was administered an equivalent volume of normal saline (Lot No. DAJ9074, DAJ9076).
All animals were observed daily for clinical signs throughout the treatment period. Abnormal signs were recorded individually by type, observation day and time and duration. The body weight of each rat was measured at the beginning of treatment and once a week during the treatment period. The amounts of food and water were measured before it was supplied to each cage and the remnant was measured on the next day. The differences were calculated and regarded as the daily food and water consumptions. On the scheduled day of study termination, all surviving animals were anesthetized by using ether inhalation. Blood samples were collected and postmortem examinations were performed on all animals. Absolute organ weights were calculated for the following organs:brain, pituitary gland, heart, lungs, liver, spleen, kidneys, adrenal glands, testes, prostate, ovaries, and uterus.
External eye examinations of the animals were carried out during the last week of the treatment period (5 rats/ group). After the administration of the Ocu-Tropic ophthalmic drops (Lot No. 019196, Samilpharma. Co., Ltd., Seoul, Korea), the conjunctiva, cornea, lens, iris and fundus of each eye were examined using an opthalmoscope (ALL PUPIL Ⅱ, Keeler, Windsor, UK).
The animals were fasted overnight prior to necropsy and blood collection. Blood samples were drawn from the abdominal aorta by using a syringe needle under ether anesthesia. Blood samples were collected into CBC bottles containing ethylenediaminetetraacetic acid (EDTA) and were analyzed to determine the red blood cell count (RBC), hemoglobin concentration (Hb), hematocrits (Ht), mean corpuscular cell volume (MCV), mean corpuscular cell hemoglobin concentration (MCHC), platelet count, white blood cell count (WBC), differential WBC count, reticulocyte count, prothrombin time (PT) and active partial thromboplastin time (APTT).
For serum biochemistry analysis, blood samples were centrifuged at 3,000 rpm for 10 minutes and analyzed using an auto-analyzer (7080, HITACHI, Tokyo, Japan). Serum biochemistry parameters including sodium, potassium, calcium, chloride, glucose, total cholesterol, blood urea nitrogen (BUN), creatinine, total protein (TP), albumin, total bilirubin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and albumin/globulin ratio were examined.
During the last week of treatment, urinalysis (5 rats/ group), were conducted on fresh urine by using a Combur10Test ®Mstick (MIDITRON®JuniorII, Roche, Manheim, Germany) to assess specific gravity, pH, protein, glucose, ketone body, bilirubin, and occult blood.
The following tissues were obtained and weighed (absolute and relative organ weights) from all animals: brain, pituitary gland, thyroid and parathyroid glands, thymus gland, trachea, heart, lungs, liver, spleen, kidneys, adrenals, testes, prostate, ovaries, uterus, salivary glands, stomach, duodenum, jejunum, ileum, cecum, pancreas, epididymis, seminal vesicles, urinary bladder, sub-mandibular lymph node, eyes, harderian glands, skin, bone marrow (femur and sternum), tongue, spinal cord, and injection site. Eyes and testes were preserved in Davidson’s fixative and Bouin’s fixative, respectively. These tissues were then fixed with 10% neutral buffered formalin solution. The tissues were routinely processed, embedded in paraffin and sectioned into 3 - 5 μm pieces. The sections were stained with hematoxylin and eosin (H&E) for microscopic examination. All organs and tissues taken from all animals in the control and the high-dosage groups were examined microscopically. In the case of pathological findings in specific organs in the high-dosage group, the low and medium-dosage groups were also examined microscopically.
Data on animal and organ weights, amounts of food and water, amount of urine, CBC, and serum biochemistry were tested using SAS (version 9.1.3, SAS Institute, Inc, Cary, NC, USA). The variance in the numerical data was checked using the Bartlett test [19]. If the variance was homogeneous, the data were subjected to a one-way analysis of variance (ANOVA). If either of the tests showed a significant difference between the groups, the data were analyzed using the multiple comparison procedure of the Dunnett’s test [20]. If not, they were analyzed using the Kruskal-Waillis non-parametric ANOVA test (
No treatment-related mortality occurred in animals treated with any dose of the SBV during any part of the experimental period.
Gait disturbance was observed in 1 case in the low-dosage group (0.07 mg/kg) on the 3rd day and the 19th day of the 13 weeks period. In the medium-dosage group (0.14 mg/kg), gait disturbances were observed in 5 - 9 cases immediately to 10 minutes after administration of the SBV. In the high-dosage group (0.28 mg/kg), gait disturbances were observed in 14 cases immediately to 10 minutes after administration of the SBV (See Supplementary Table 1)
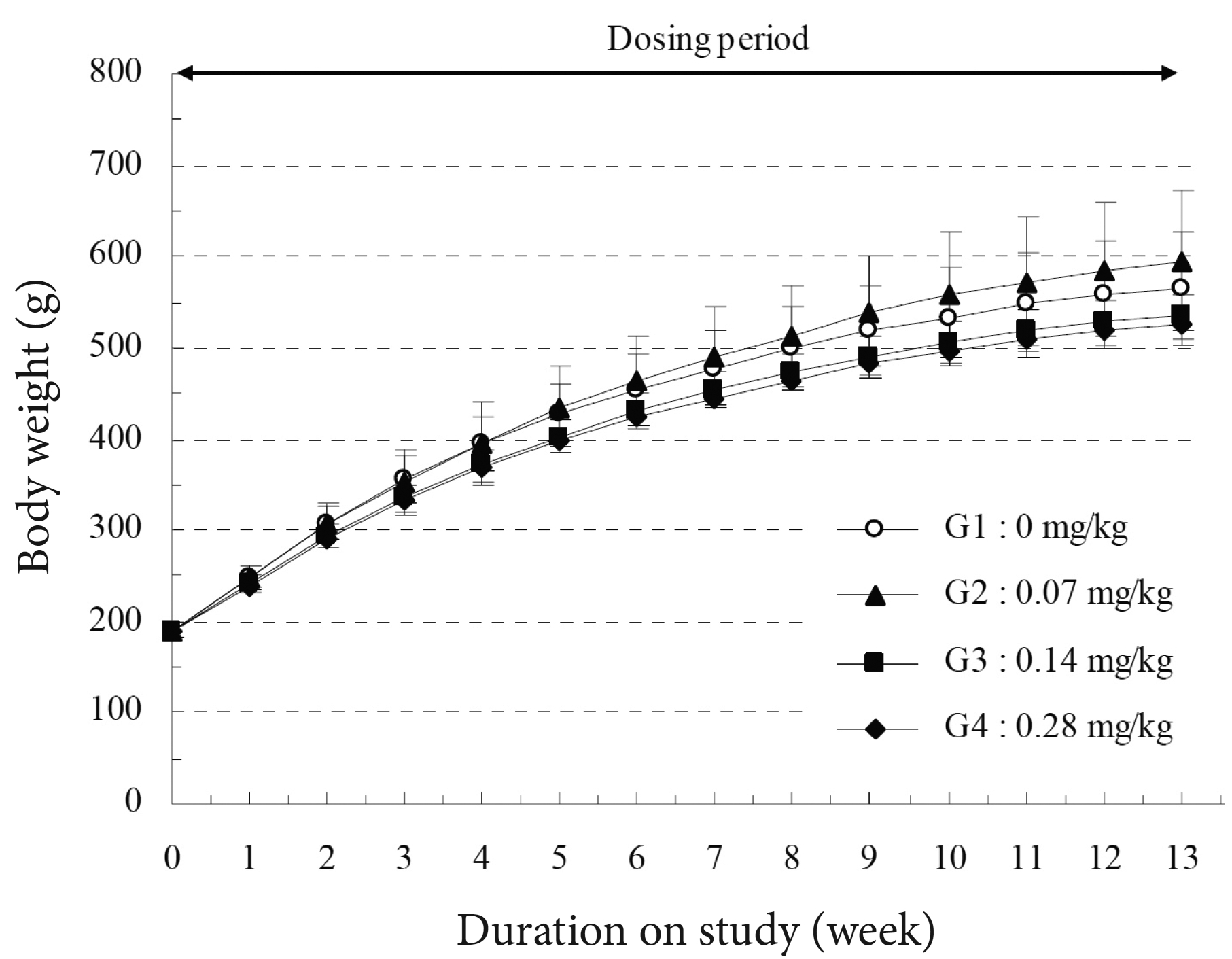
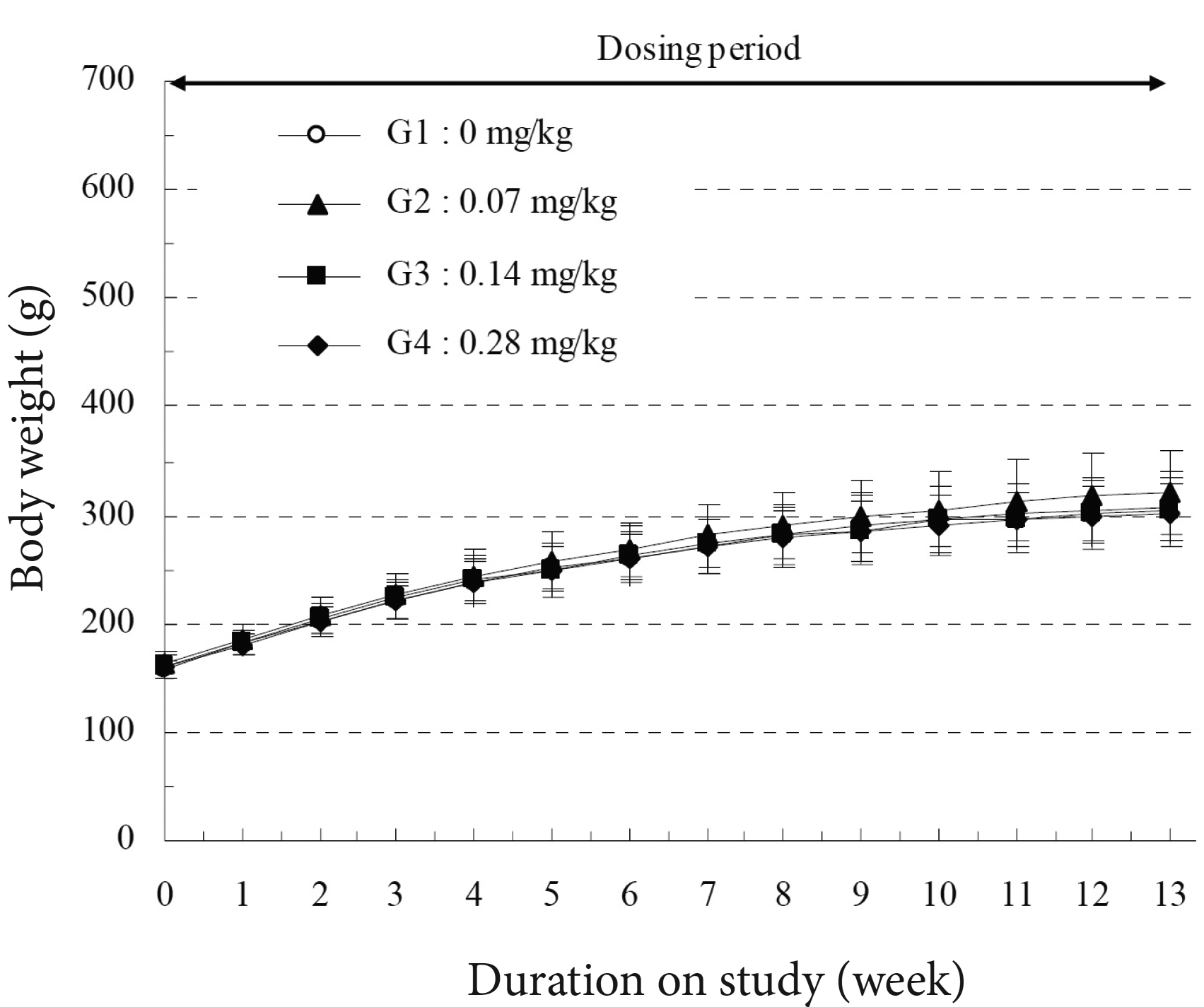
As shown in (Fig 1, 2 and Supplementary Table 2), the high-dosage (0.28 mg/kg) male group showed a significant decrease in body weight during 2 to 4 weeks of treatment period, but the female group did not show a significant change in weight. The control and the experimental groups showed normal amount of food and water (Supplementary Table 3).
Compared to the control group, no experimental groups showed any significant changes in the parameters measured during the ophthalmic examination (Supplementary Table 4).
In both the control and the experimental groups, ketone bodies and occult blood were observed in the urine in some cases; these symptoms were not related to the toxicity. In the 4-week recovery period, no experimental groups showed any significant changes in the urinalysis parameters compared to the control group (Supplementary Table 5).
Hematology studies revealed that the high-dosage (0.28 mg/kg) male group showed significant delays in prothrombin time (PT) but females exhibited no significant changes compared to the control group. The high-dosage (0.28 mg/kg) female group showed a significant increase in eosinophils but the mean value was very small and was not considered to be due to any toxic effect (Supplementary Table 6) Serum biochemistry revealed that the medium and the high-dosage male groups showed a significant decrease in total bilirubin and albumin concentrations. The high-dosage male group showed a significant decrease in total cholesterol, total protein, and Ca values but the mean values were so small that they were not considered to be due to toxic effects (Supplementary Table 7).
In the measurements of absolute organ weights, the high-dosage male group showed a significant decrease in liver weight, but the female group did not show any significant change, compared to the control group.a
In the measurements of relative organ weights, the high-dosage male group showed a significant decrease in the liver weight and the high-dosage female group showed significant increases in heart and lung weights compared to the control group. The medium-dosage female group showed significant changes in kidney and adrenal gland weights compared to the control group (Supplementary Table 8 and 9).
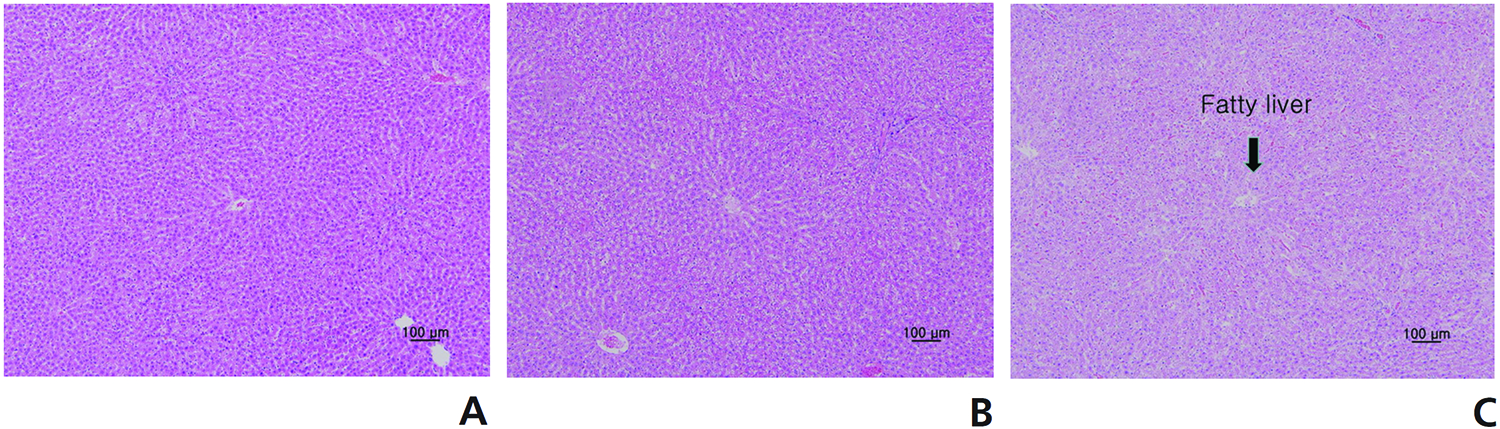
Supplementary Table 10 and 11 summarize the results of the histopathological examinations. Examinations of the thigh muscles, into which the SBV had been injected, showed cell infiltration, inflammation, degeneration, and necrosis of muscle fiber, as well as fibrosis, in the low-, medium-, and the high-dosage groups (Fig 3). The medium- and the high-dosage groups showed some fatty liver changes in the periportal area (Fig 4). No abnormalities were observed in any other organs.
The primary known pharmacological action of BVP is stimulation of the hypothalamic-pituitary-adrenal axis to increase the secretion of adrenocortical hormone. BVP thus possesses strong analgesic and anti-inflammatory actions. Bee venom contains enzymes with molecular weights greater than 10,000 such as phospholipase A2 and hyaluronidase. These proteins act as antigens, causing allergic reactions. Low molecular weight substances such as histamine cause itching and inflammation. Hence, one of the biggest obstacles in using BVP clinically is allergic reaction. The most concerning reaction of BVP is a systemic immediate reaction (anaphylactic shock). Some of the symptoms seen under this condition include an extensive accentuation of vasopermeability, dizziness from a drop in blood pressure, syncope, and unconsciousness. This is the most severe type of hyper-sensitivity, and taking a rest and drinking warm water will induce the symptoms to subside. However, if the blood pressure drops below 90/60 mmHg with tachycardia of over 120 beats/minute, the condition is emergent and needs to be addressed accordingly [1].
SBV was developed to overcome the problems of BVP [21, 22], and SBV had been reported to have fewer allergic responses than BVP and to be as effective as or better than BVP [12, 23].
In previous studies on SBV, Kwon et al. and Yoon
We evaluated the toxicity of SBV in SD rats based on a 13- week, repeated dose test to ascertain the NOAEL dosage of SBV. No treatment-related mortalities occurred in the animals treated with any dose of SBV during the experimental period. Some experimental groups showed gait disturbances, particularly at higher doses of SBV. However, this symptom lasted for only 10 minutes after the injection.
A significant decrease in body weight was observed in the high-dosage (0.28 mg/kg) male group, but not in the female group. Significant changes were observed in the ophthalmic examination, urinalysis, hematology, and serum biochemistry of the treated groups, compared to the control group. However, these changes were not considered to be due to any toxic effects of SBV.
Some changes in organ weights were observed in the medium- and the high-dosage groups, but the low-dosage group did not show any significant changes, compared to the control group.
Histopathological examinations revealed some fatty liver changes in the periportal area in the medium- and the high-dosage groups. Examinations of the thigh muscles into which the SBV was injected revealed cell infiltration, infammation, degeneration, and necrosis of muscle fiber, as well as fibrosis, in all experimental groups. We think these changes are temporary and reversible, but a recovery test should be conducted to verify that
We estimate that the NOAEL of intramuscular injection of SBV is 0.07 mg/kg in male and female rats and that the observed histological changes in the thigh muscle and liver in the medium- and the high-dosage group are reversible. Because the dosage of SBV commonly used clinically is very much lower than 0.07 mg/kg, we, conclude that the current clinical use of SBV is safe. Further studies should be conducted to yield more concrete results.

![Thigh muscle tissues from SD rats that participated in a 13-week, repeated intramuscular dose, toxicity study. The rats in the (A)
low-dosage group, the (B) medium-dosage group, and the (C) high-dosage group showed degeneration, fibrosis, inflammation, panniculitis,
and necrosis of muscle fiber, and the severity of these changes was greater in the rats in the high-dosage group. These results show that Sweet Bee
Venom has an effect on muscle fiber. Pathological changes were detected by using hematoxylin & eosin (H&E) staining (× 200 [A, B, C]). The stars
show degeneration of muscle fiber, the small arrows show regeneration of muscle fiber, the big arrows show inflammatory cell infiltration and
the crosses show fibrosis.](http://oak.go.kr/repository/journal/13092/DHOCBS_2014_v17n2_73_g003.jpg)