Dysmenorrhea, spasmodic or congestive is the most frequently occurring symptom, for which women consult gynecologist. Every woman experiences this pain, more or less in her life. The cause for primary dysmenorrhea is yet to be established while secondary dysmenorrhea is due to some pelvic pathology and hence is curable. The pain in primary dysmenorrhea is attributed to uterine ischemia, release of prostaglandin, vasopressin and forceful irrhythmic contraction of uterus (Akerlund et al., 1995; Bossmar et al., 1995; Kennedy, 1997; Rosenwaks and Seegar-Jones, 1980). In some women severity of the pain is sufficient enough to enforce them for absence from work place or school. (2, 36) Dysmenorrhea is taken differently by different socio economic groups and so is response and reporting. Because of this, different social groups present variable statistics. The overall prevalence of dysmenorrhea is reported to be 28% (Loto et al., 2008).
Risk factors associated with dysmenorrhea are increase age, early age at menarche, parity, longer menstrual cycles, increase duration and amount of flow, smoking, alcohol consumption, diet, body weight, physical activity, positive family history and psychological etc (Andersch and Milsom, 1982; Banikarim et el., 2000; Balbi et al., 2000; Juang et al., 2006; Klein and Litt, 1981).
It is hypothesized that an earlier start to reproductive life in some way decreases the sensitivity of the uterus to prostaglandin. But there is also the possibility that those who had a relatively earlier birth of first child have relatively higher progesterone levels. The other hypothesis is that higher level of prostaglandin is a risk factor for miscarriage. In this case, women with higher levels of prostaglandin and or higher sensitivity to them could have given their first live birth relatively later (Rosenwaks and Seegar-Jones, 1980; Weissmann et al., 2004).
In several studies higher prevalence of dysmenorrhea with early onset of menarche and in teen age is attributed to anovulatory cycles (Bossmar et al., 1995; Rosenwaks and Seegar-Jones, 1980). Decreasing trend of dysmenorrhea with advancing age has been reported (Weissman et al., 2004). Contrary to earlier belief studies confirmed unresponsiveness of Dysmenorrhea to vaginal delivery and to pregnancy. Age dependency of Dysmenorrhea has been shown in many studies as in multiparous women severity of pain decreased after the age of 40 years (Ju et al., 2010). Longer or irregular menstrual cycles (Zukri et al., 2009) and longer duration of menstrual flow (Solomon et al., 2013) also cause menstrual pain. Postponing the start of reproductive life to mid twenties is a mean that the number of menstrual cycles for women with earlier menarche is quite high. Thus, the period of time between first menstruation and conception might be a better predictor of menstrual pain in parous women than the age of menarche itself. The length of time after puberty in which uterus is exposed to prostaglandins and the number of menstruations can influence the prevalence of menstrual pain in adult reproductive life, but pregnant or lactating women experienced a less number of cycles (Sterasam, 1997).
To investigate the associated risk factors that could influence menstrual pain.
The present Cross Sectional Study was conducted at Dept. of OBG, National Institute of Unani Medicine, Bangalore during the year of 2014. The study consisted of 230 women with the ages between 20 - 49 years with complaint of dysmenorrhea. All newly married, nulliparous and parous women were included. The detailed reproductive history like age, age at menarche, duration of cycle, duration and amount of flow, pain during menstruation and its intensity and number of abortions, number of pregnancies were recorded. Some women could not reveal the information about their menstrual symptoms or age of menarche. The collected data were analyzed statistically.
Cross sectional study.
2 months.
230.
>
Method of collection of data
By history.
All married women complaining of pain abdomen during menstruation.
Menopausal women.
The present study was conducted to observe the relationship between dysmenorrhea and associated factors whether they relieve the dysmenorrhoic pain or not. The study consisted of 230 cases of dysmenorrhea. The data observed were as:
Age has a significant effect on the severity of dysmenorrhea. Older women are more like to experience less severity and prevalence of dysmenorrhea. Primary dysmenorrhea frequently occurs in women aged 15 - 24 years and then declines as women age advances to 25 to 34 years (Walraven et al. 2002). Similarly the international association of the study of pain reported that primary dysmenorrhea is most common between ages of the 15 - 19 years and declines thereafter.
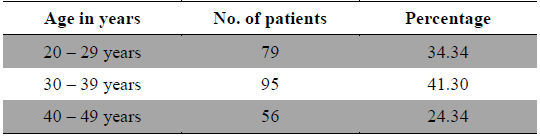
The present study revealed that according to age distribution analysis this disease was prevalent throughout reproductive life i.e. 20 - 49 years of age, but higher prevalence was observed in middle age i.e. 30 - 39 years (Table 1) and it was concordant with the finding of Weissman et al. (2004). Out of 230 cases of dysmenorrhea 79 cases were between the age of 20 - 29 years, 95 cases were between 30 - 39 years of age and 56 cases were between 40 - 49 years of age (Table1), in a longitudinal study of the natural history of Primary Dysmenorrhea it was reported that older age was associated with less severe dysmenorrhea (Walraven et al. 2002). Furthermore in another study found that the severity of primary dysmenorrhic pain decreased significantly after the age of 40 years in nulliparous women (Juang et al., 2006)
[Table 1.] Age wise distribution of patients.
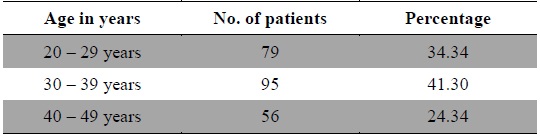
Age wise distribution of patients.
In their study Rebecca et al. and Harlow and Park concluded that it is an age related disease and that the symptoms gradually decrease with increase in age. The incidence also tends to decrease with age (Harlow and Park et al., 1996).
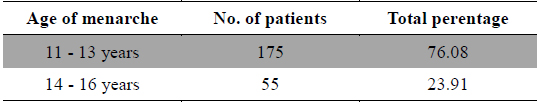
Studies on the prevalence of menstrual pain have shown that many factors are related to this disorder. The relationship between age at menarche and dysmenorrhea is contradictory. In present study it was observed that out of 230 cases 175 cases were found between the age of menarche of 11 - 13 years (Table 2) and this finding was concordance with the finding of Andersch and Milsom (1982). In their study they documented that early age at menarche was associated with an increase in the severity and duration of dysmenorrhea (Harlow and Park, 1996; Montero et al., 1999; Patel et al., 2006; Pawlowski, 2004). Conversely Derman et al. (2004) could not observe clear relationship between age at menarche and dysmenorrheal.
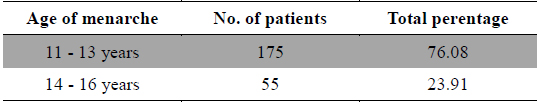
Age of Menarche.
>
Duration and amount of menstrual flow
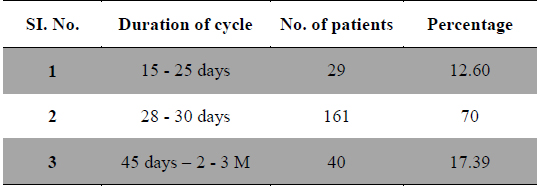
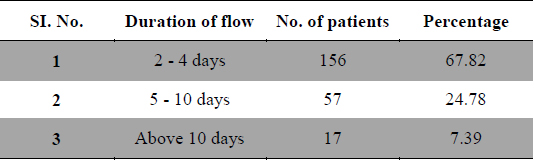
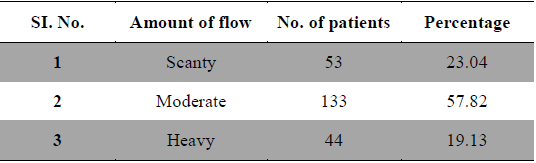
Duration and amount of menstrual flow as risk factor for dysmenorrhea are controversial. Longer or irregular menstrual cycles (Derman et al., 2004) and duration of menstrual flow (Montero et al., 1999) also cause menstrual pain. In present study 29 patients had frequent cycles, 161 patients had normal length of cycles and 40 patients had longer menstrual cycles (Table 3). Regarding the duration of flow 156 patients had 2 - 4 days of flow, 57 patients had 5 - 10 days and 17 patients had more than 10 days of menstrual flow (Table 4), whereas 53 patients had scanty flow, 133 patients had moderate flow and 44 patients had heavy menstrual flow (Table 5). According to many studies long and heavy menstrual flow has been associated with an increased risk of dysmenorrhea (Solomon et al., 2002). Conversely, Tangchai et al. (2004) reported that dysmenorrhea was not associated with the duration of the menstrual cycle and amount of bleeding in each cycle. In some studies severity of pain has been correlated with menstrual flow (Vink et al., 2006).
[Table 3.] Duration of menstrual cycle.
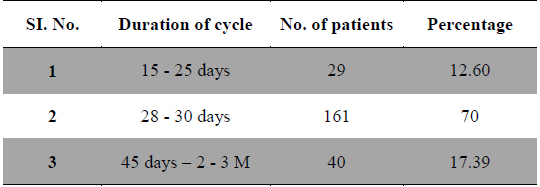
Duration of menstrual cycle.
[Table 4.] Duration of menstrual flow.
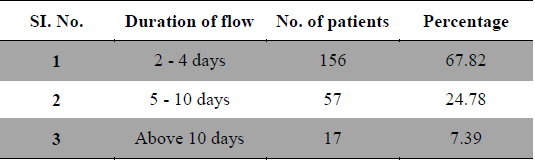
Duration of menstrual flow.
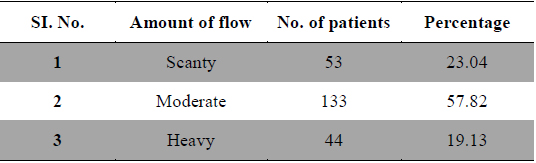
Amount of flow.
Epidemiological studies have revealed so many associated factors responsible for dysmenorrhea. Primary dysmenorrhea occurs more frequently in unmarried than in married even of advanced age (61% versus 51% respectively). Although primary dysmenorrhea tends to improve and to decrease with age more rapidly in married than in unmarried women and pregnancy, vaginal delivery do not necessarily cure it (Klein and Litt, 1981).
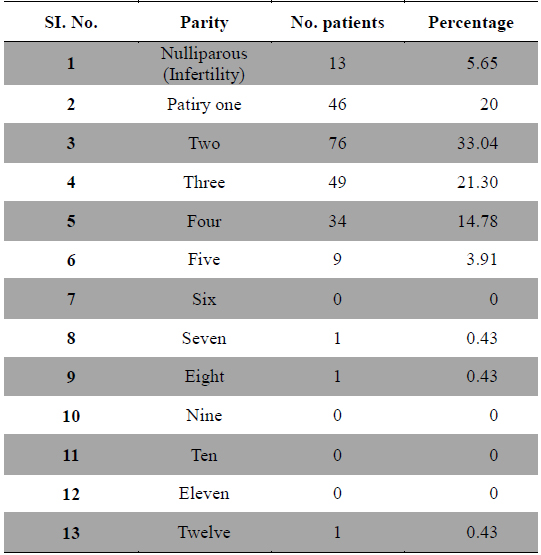
Childbearing is said to relieve dysmenorrhea, but this does not always occur. One study revealed that in nulliparous women with Dysmenorrhea, the severity of menstrual pain decreased significantly after the age of 40 years (Vink et al., 2006). Another study indicated that dysmenorrhea was present in 36.4% of participants and was significantly associated with lower age and lower parity (Juang et al., 2006). In other study it was reported that parity also plays a role. Both the prevalence and severity of Dysmenorrhea reduced after the first delivery and in women who were parous than women who had never been pregnant or women who had experience a medical or spontaneous abortion (Solomon et al., 2002; Sundell et al., 1990; Weissmann et al., 2004). Regarding the parity in present study out of 230 cases 60 patients had a history of abortion, 13 were nulliparous, 46 were of parity one, 68 were of parity two, 49 were of parity three, 34 were of parity four, 09 were of parity five and only one case each was found of parity seven, eight, twelve and no patient was found of parity six, nine, ten and eleven (Table 6). Out of 230 cases severe dysmenorrhea was found in patients of parity one, moderate dysmenorrhea was seen in patients with parity two to four, whereas mild dysmenorrhea was seen in patients of parity five and above as the prevalence of high parity was also low. Often primary dysmenorrhea becomes of less severe with age or after childbirth (Andersch and Milsom, 1982; Wong et al., 2009). Parity was also reported negatively related to dysmenorrhea from Singapore (Ng et al., 1992) and from Poland (Skierska et al., 1996).
[Table 6.] Dysmenorrhea and parity.
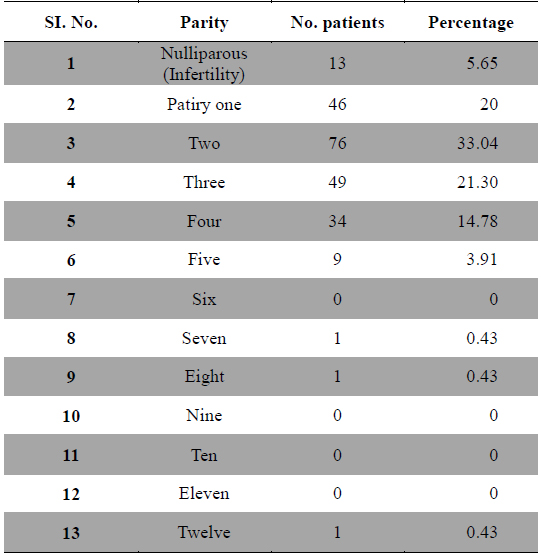
Dysmenorrhea and parity.
The present study was carried out to observe how the Dysmenorrhea is associated with risk factors like age, age at menarche, menstrual cycle irregularities, parity etc. It was observed that early age at menarche increases severity and duration of menstrual pain, whereas its prevalence decreases with advancing age and parity.
On the basis of the above observation, it is concluded that large sample would accurately determine strength of the association of under study risk factors with Dysmenorrhea.