Many patients with psoriasis look for treatment options other than conventional treatment to control their disease with less side effects. We evaluated the prevalence and characteristics of herbal therapy usage among patients with psoriasis in Turkey. A self-prepared questionnaire about herbal therapies was applied to the psoriatic patients attended our dermatology clinic between October 2013 and December 2013. A total of 100 patients (55 male, 45 female; 7 - 80 years of age) were included in this study. Fortynine percent of patients used at least one form of herbal therapies. Juniperus oxycedrus and Aloe vera were found to be the most frequently used plants. 36.7% of the patients get benefit from herbal therapy. Only 12.2% of patients had informed their clinicians during or after herbal therapy usage. 22.4% of the patient had continued conventional treatment during herbal therapies. Side effects related with herbal therapy were developed in 26.5% of the patients. The risk of side effects was found to be 5.23 times more in patients using phytotherapies systemically compared with ones using topically. Our results show that herbal therapy usage is common among patients with psoriasis in Turkey. Since herbal therapies have the potential of interacting with the medical treatment modalities and causing life threatening allergic reactions, clinicians should be aware of plants used in psoriasis and possible adverse reactions related with them and also should not forget asking about herbal therapy history.
Psoriasis is a common, chronic, recurrent and immune-mediated inflammatory disorder characterized by circumscribed, red, thickened plaques with an overlying silver-white scale (Schön and Boehncke, 2005). Conventional topical and systemic treatments of psoriasis are based on severity of the disease (Traub and Marshall, 2007). In addition to risk of side effects that topical and systemic treatments carries, disease generally recurs in a short period of time after cessation of therapy (Yuqi, 2005). Also, the visible nature of psoriasis brings additional psychosocial burden and patients may wish to do anything to heal their disorder as soon as possible. So, many patients with psoriasis look for another treatment options to control their disease with less side effect.
Phytotherapy, which means treatment with products prepared from herbs, spices, roots, stems or other parts of fresh or dried plants or exracted plant material (Reuter et al., 2010), was reported as the most frequently used complementary and alternative medicine modality among patients with psoriasis (Gönül et al., 2012). Herbal therapies are greatly accepted by the patients because they are believed to be safer than conventional therapy. Actually, many of these products lack evidence of safety and efficacy. In the realm of increasing popularity of herbal therapies, clinicians should be aware of current scientific data about these products.
The aim of this study is to investigate the prevalence and characteristics of herbal therapy usage, self beliefs about herbal therapies and factors influencing the use of herbal therapies among patients with psoriasis in Turkey.
The study included 100 psoriatic patients successively attending our dermatology clinic between October 2013 and December 2013. Patients were examined by dermatologist and patients whose diagnoses confirmed histopathologically included the study. The study was approved by the local medical ethical committee. All participants were informed about the aim of the study and provided written consent prior to their interviews.
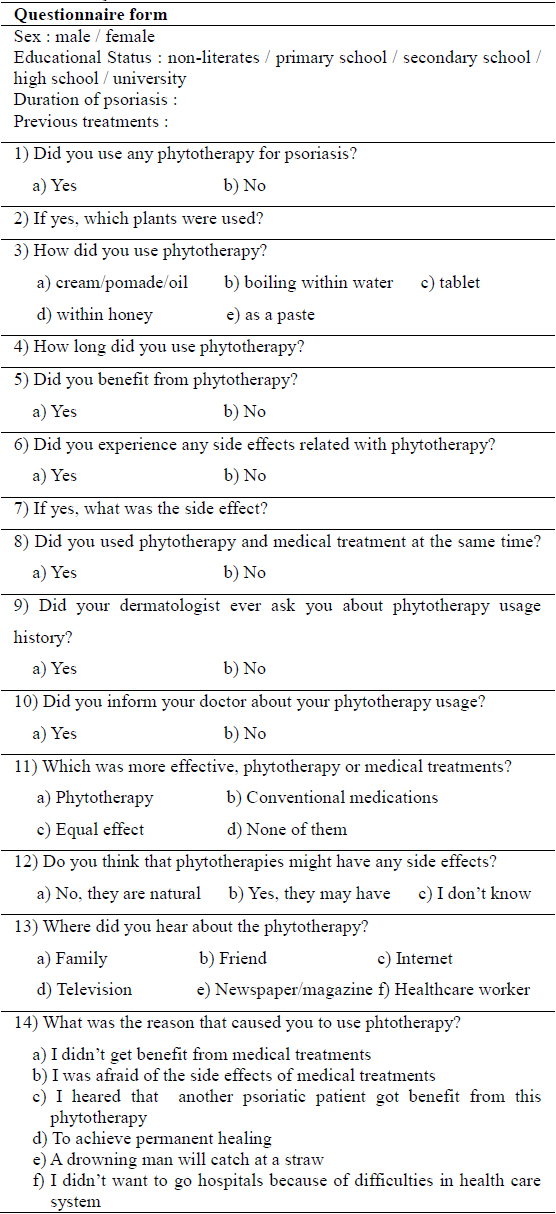
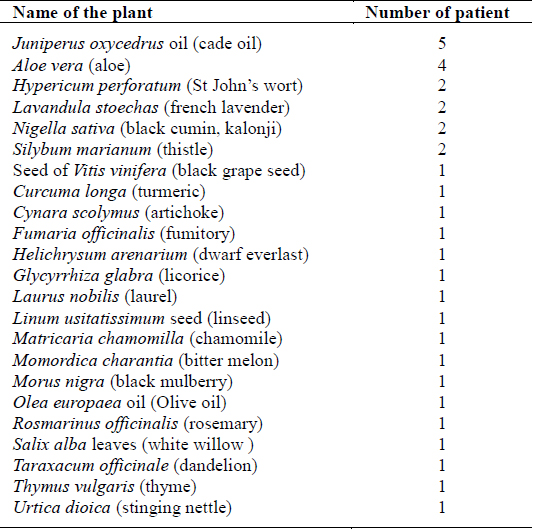
The main descriptive features of patients (the age, sex, education status), the duration of psoriasis and the previous treatments that patients used were recorded. A self-prepared questionnaire about herbal therapies was applied to the patients with face to face interview technique. The questionnaire form was prepared by researcher after reviewing the literature about this topic. The questionnaire explored the participants’ experience and attitude towards phytotherapy in psoriasis treatment. The questionnaire form was shown in Table 1.
Questionnaire Form
The ages of the patients were grouped as under 25, 26 - 40, 41 - 60 and over 60 years. The education status was classified into two groups: non-literates and graduated from primary school in one group and graduated from secondary school, high school and university in the other group. The duration of psoriasis was grouped as under 1, 2 - 10, 11 - 20 and over 21 years. The forms of phytotherapy were classified into two groups: externally used cream, pomad and oil forms were and orally used paste, tablet, drinks after boiling were classified as systemic ones. Also, the side effects were classified into two groups: related with skin and systemic ones. Side effects related with skin were further divided into two grups: exacerbation of lesions was classified as localized skin side effects and erythema, pruritus, burning, stinging, angioedema, urticaria were classified as generalized skin side effects. Stomach pain, leg oedema, increase in blood glucose were classified as systemic side effects.
Data analysis was performed by using the SPSS statistical package. The relationship between phytotherapy users and nonusers and cathegorical variables such as sex, age, educational status were examined by using the chi-square test.
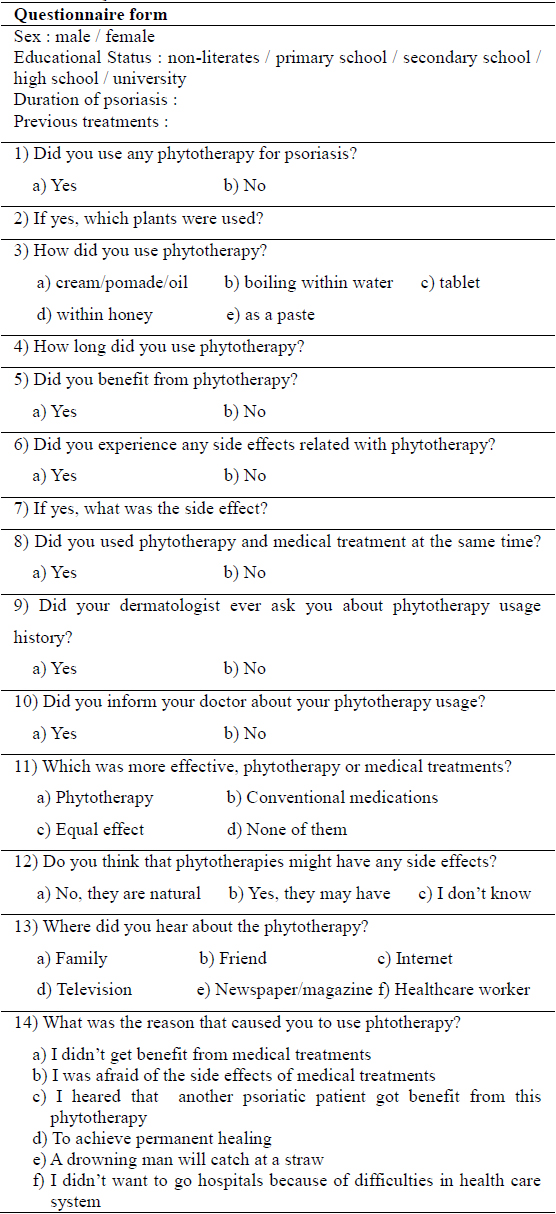
One hundred psoriatic patients were enrolled in the study: 55.0 % were males and 45.0% were females. The mean age of patients were 44.88 ± 15.17 years (minimum 7, maximum 80 years). The demographical charactheristics of patients were summarized in Table 2. Although female patients were found to be using phytotherapies for psoriasis more frequently than males (55.56% vs 43.64%), the difference between both groups did not reach statistically significant level (
[Table 2.] Demographical charactheristics of patients
Demographical charactheristics of patients
Fortynine percent of patients (n = 49) used at least one form of herbal therapies. While 35.1% of the phytotherapy usage was in the form of topical application, 32.4% as drinks that prepared with boiling within water, 17.6% in tablet form, 6.8% as mixture within honey and 8.1% were in paste form to eat.
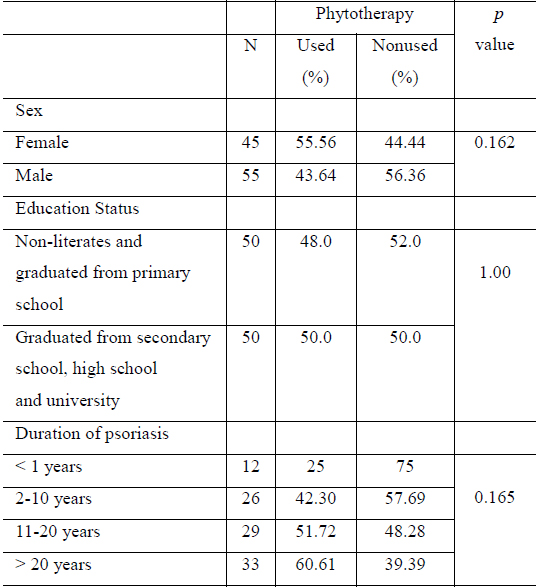
46.9% of the patients didn’t know or couldn’t remember the name of the plant(s) they used. Among the remaining 53.1 % of patients,
[Table 3.] The list of plants used and the number of patients using these
The list of plants used and the number of patients using these
36.7% (n = 18) of the patients got benefit from herbal therapy. Among them, only 4 patients stated that herbal therapies were more effective than conventional therapies. But, the major proportion of them (66.67%, n = 12) found conventional therapies more effective. 75.51% (n = 37) of the phytotherapy users believed that conventional therapies are more effective than the herbal therapies. Other beliefs were as follows: 10.20% (n = 5) herbal therapies more effective, 6.12 % (n = 3) equal effect, 8.16% (n = 4) neither conventional nor herbal therapies effective.
Side effects related with herbal therapy were developed in 26.5% (n = 13) of patients using phytotherapy. In 10 patients skin related side effects, in 7 patients systemic side effects and in 4 patients both side effects were developed. The most frequent side effect was increase in number of lesions (n = 6). The other side effects seen in the patients were as follows: stomach pain (n = 5), erythema, pruritus and burning (n = 3), angioedema (n = 1), leg oedema (n=1) and increase in blood glucose (n = 1) (Table 4). The risk of side effects was found to be 5.23 times more in patients using phytotherapies systemically compared with ones using topically (
[Table 4.] Side effects, name and administration way of plant
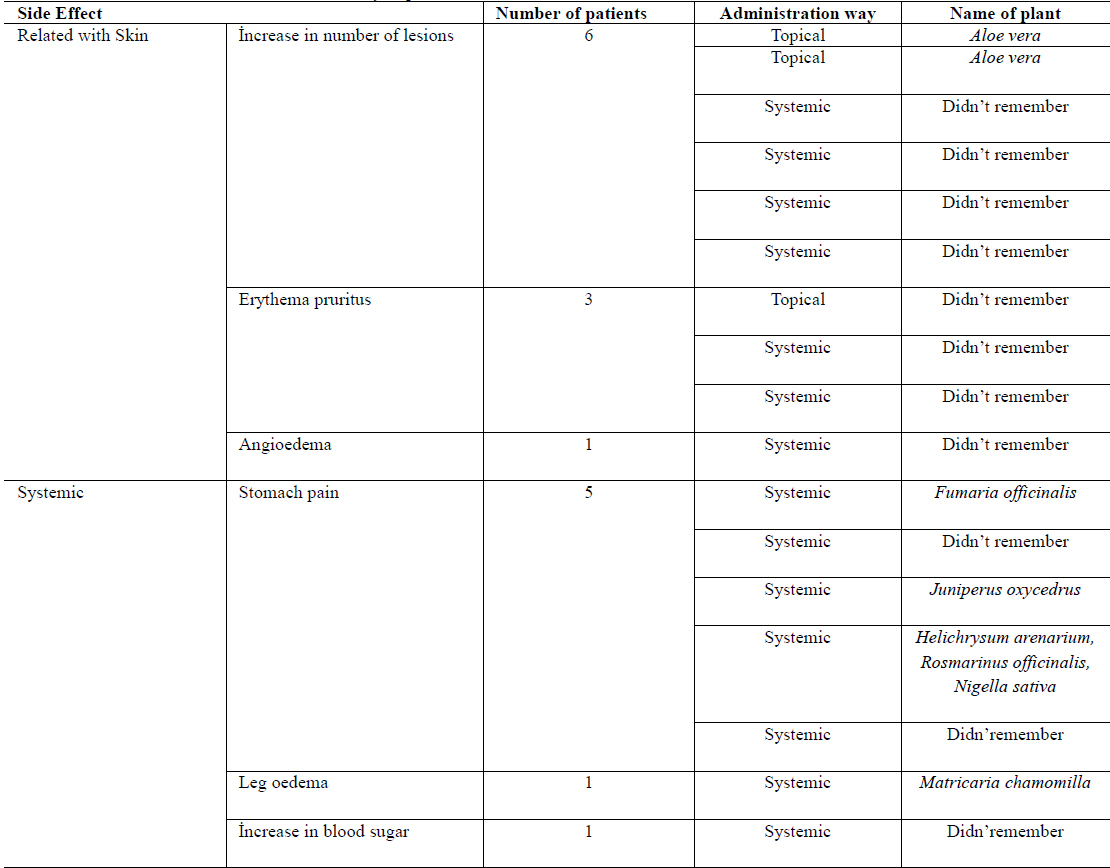
Side effects, name and administration way of plant
Among 49 patients using phytotherapy, only 12.2% (n = 6) had informed their clinicians during or after herbal therapy usage. It was found that only 10.8% of clinicians (n = 5) had asked their patients about herbal therapy history. The 22.4% of the patients (n = 11) had kept on conventional treatment with herbal therapies. The rate of side effect was found to be higher among patients using both therapies together than patients using phytotherapies alone (36.36% vs 23.68%).
We asked patients whether phytotherapies might have any side effects or not? If we exclude 13 patients who experienced side effects of phytotherapy, 39.02% of the remaining patients said ‘Yes, it could be’, 30.48% said ‘no, plants are safe because they are natural’, 30.48% said ‘no comment’. Among patients who answered as yes, 53.12% used phytotherapy despite the possible risk of side effects.
When we asked patients from where they heard about the name of herb they used, 45.28% of patients advised by friends, 28.30% by tv/radio, 15.08% by family members, 5.66% by internet, 5.66% by health care worker other than dermatologist.
When we asked the reason for using phtotherapy, 52.94% of the patients answered that they couldn’t get benefit from conventional therapies. The other answers were as follows: ‘beneficial effects of the herb on another patient with psoriasis’ (19.60%), ‘ to achieve permanent healing’ (9.80%), ‘fear from side effects of conventional medications’ (7.84%), ‘ a drowning man will catch at a straw’ (5.88%), ‘difficulties in health care system (3.92%).
The frequency of complementary and alternative medicine use among patients with psoriasis was reported to be between 43%-69% in the literature (Smith et al., 2009). Although data on herbal therapy use in psoriasis is relatively sparse, herbal therapies were reported as the most frequently used complementary and alternative medicine modality among patients with psoriasis (Gönül et al., 2012). Our study showed that 49% of patients with psoriasis used at least one form of herbal therapies. This rate is high when compared with that found by Gönül et al. (Gönül et al., 2012) (24.1%) but comparable with that found by Ben-Arye et al. (Ben-Arye et al., 2003) (40.3%). In two recent study, herbal therapy usage was found to be 16.6% between diabetes mellitus patients (Wazaify et al., 2011) and 7.6% between chronic kidney disease, dyslipidemia and hypertension patients (Wazaify et al., 2013). Although, the patients in both studies had chronic disease, the prevalence of herbal therapy usage was found to be lower in omparison with psoriatic patients. This difference could be explained by visible nature of psoriasis. Because of the visible nature of psoriasis, patients might feel the need for another treatment options to achieve lesion free period as soon as possible.
No significant relationship was found between phytotherapy use and sex, educational status and duration of disease of the patients when compared statistically. No studies have been done to investigate the phytotherapy usage among patients with psoriasis in Turkey but Gönül et al. found no significant relationship between unconventional treatment use and educational status, duration of disease but they found significant relationship between unconventional treatment use and male sex (Gönül et al., 2012).
The
Side effects related with herbal therapy were developed in 26.5% (n = 13) of patients. The most frequently seen side effect was increase in number of lesions (n = 6). This data point out that although patients used these therapies in an effort to heal completely, the condition might become even worser in some cases. Another important point is that two of these cases had developed after topical
Herbal therapies are greatly accepted by the patients because they are believed to be safe due to their natural origin (Reuter et al., 2010). In our study, only 39.02% of the patients agreed that herbal therapies could cause side effects. But, among them 53.12% used phytotherapy despite the possible risk of side effects. This result once more emphasize that patients with psoriasis desparately could try anything to heal.
Similar to previous studies (Durusoy et al., 2010), most of the patients used phytotherapy according to advise by friends and family members (45.28% and 15.08%, respectively). The second frequent inducer was found to be advertisement in telecommunication devices like tv/radio (28.30%). We believe that advertisement of herbal product should include a warning like ‘Do not use without asking your clinician’ to improve the awareness about herbal therapies in order to decrease possible side effects and life threatening drug interactions.
We found that the lack of satisfactory treatment (52.94%) was the most important reason why patients try phytotherapies. The cure expectancy of patients during conventional therapies might cause dissappointment in time. Actually, psoriasis is not a totally curable disease because of its chronic relapsing nature, so the aim of the treatment is to provide only remission (Traub and Marshall, 2007). If this fact is explained clearly to the patient thoroughly at the beginning, concordance to the treatment and confidence to the clinician will increase and patients don’t need to search for another treatment options.
It was reported that most of the patients don’t mention about herbal therapies they used during visits and sometimes clinicians forgot asking herbal therapy usage in history (Ben-Arye et al., 2003). In our study it was found that only 12.2% of their clinicians during or after herbal therapy usage and only 10.8 % of clinicians had asked their patients about herbal therapy history. While some patients replaced standard (36.36% vs 23.68%). Therapies with herbal therapies, 22.4% of the patients combined conventional treatments with herbal therapies in an effort to do everything possible to heal as soon as possible. These rates point out the importance of asking about the use of herbal therapies while taking patient drug history.
Herbal therapies have become increasingly popular over the past decade. But, there is still conflicting evidence about safety and efficacy of herbal therapies in psoriasis. Although it was believed that herbal products are ‘natural’ and thus ‘safe’, life threatening allergic reactions or drug interactions may occur. This study emphasized the widespread use of herbal therapies among psoriatic patients in Turkey. Whatever the patients’ age, sex and educational status, the patients with psoriasis look for new treatment options to cure completely. The