Ayurvedic fundamentals of health care present a unique understanding about the human physiology, subsequent pathology including the local and systemic ones and eventual treatment approaches on the basis of cause of the disease and also on the basis of specifications associated with the disease and the person who is suffering with the disease in an entirely individualized setting (Lurie, 2012).
Modern medicine on the basis of its understanding to the cause of disease and subsequent treatment principles appear alien to Ayurvedic fraternity and is largely criticized by Ayurvedic physicians for its segmental, reductionist and fragmentary approach. Ayurvedic fraternity claims Ayurveda to be superior to its contemporary for its inclusive, comprehensive and holistic approach, proposing that it is the whole body which requires the treatment and not a component of the body which needs to be treated (Chatterjee and Pancholi, 2011).
On the contrary, Allopathic physicians criticize ayurveda for its unproven, empirical and untested claims and often deny it to be considered as a scientific method of health care (Kaptchuk and Eisenberg, 1998).
Ironically, because of mutually contrasting viewpoints towards treatment approaches for a similar subject and with the same objective (where the patient is still the same with essentially same sufferings and has the only objective of getting away from the sufferings from whatever healthcare system it is possible), any convergence of modern medicine and Ayurveda (any traditional medicine in general) has never come to a reality. As a result, a huge sum of human population remained deprived of the best treatment possibilities which might have resulted through a logical convergence of various health care systems. An intersystem hostility has resulted into the health care benefits limited to the system of care chosen, at the cost of deprivation of the benefits which could have been offered additionally if a converged health care vision could have been adopted for a comprehensive health care (Ghodke et al., 2011).
The point we are willing to raise here is not that the different health care systems are having their own strengths and weaknesses in certain sectors and that their rational utilization on the need basis may result in optimal health care. We argue here that primarily all the health care systems are homologous and are derived to serve the primary purpose of healing the illness. Any difference which is visible in their approaches is likely to be a reflection of thought process accumulated over the historical period of their development. It is likely all of these systems are fighting against the diseases but with different weapons. And these weapons are essentially the reflection of state of the art techniques available at then times.
It is logical to argue that for one subject having a set of complaints, if similar responses are obtainable from two different treatment approaches, the actual biological process which might be causing the relief must also be same. It is simple to think that if a similar relief is there, the intervention should have affected the pathogenesis in a more or less similar way. This gives us logic to think that in whatever way we read it; the ultimate pathogenic process which might have occurred in the sick referring to the manifestation of the disease and also the ultimate therapeutic process in response to the intervention would essentially be the same irrespective of the name of the system. There can be a difference in inferring the happenings in a given case as per our established mind set of knowledge but as ultimate end point is the relief from the symptoms or cure of the disease, the eventual pathway through which the relief comes is ought to be same (Patwardhan and Mashelkar, 2009).
Ayurveda while sticking to its own traditional principles of disease understanding and being less flexible to more advanced diagnostic and treatment tools, often fails to respond effectively in many conditions where a quick relief might be required in order to save life or in order to find time to think more logically to derive a comprehensive treatment plan later on. Similarly modern medicine, by considering ayurvedic principles as irrational, unscientific and non-evidence based, remains deprived of the goodness of such wisdom which had been offering relief to the ailing humanity for past many generations in many conditions (Olivier et al., 2008). There had been the talks of integrative medicine since long. India is a unique country having the medical pluralism in real practice since long. This integrative medicine as is understood today is the utilization of many systems as per their strengths in one condition. The common integrative practice in India is choosing the sectional responsibilities in a phased manner for one patient. After one phase of treatment through one system, the patient can be handed over to other system for next phase of treatment. This is a kind of skeptical integration, we are integrating but with full of disbelief on each other and are integrating only where we fail. It’s a choice based integration where the failures are making room for some other remedies claiming to offer a cure.
What we mean is little larger than this. Our meaning of integration is integrating the way of understanding of a disease and the way we treat it. This do not mean a skinny integration but intends to be more deep giving a due space to every science involved in health care, with adoption and assimilation of the understandable principles of health care from other sciences to one’s own and giving room to all that which is not understandable now as the knowledge still to be understood.
This would have been very interesting to see how ayurvedic principles are looked at from modern logic and also the vice versa. There had been many approaches trying to see ayurvedic principles from a modern view point. We try to make a counter view of looking modern principles through an ayurvedic logic.
To a logical mind, this is much interesting to see how newer diagnostic tools and treatment principles can be deduced to an ayurvedic logic and how they can help enriching ayurveda by adding up to its own principles.
Thinking this way would not only empower ayurveda and its practitioners to be better equipped but at the same time would also be helping the patients to find the best possible and timely cure without wasting much of their resources. Following is a case report where the modern treatment approach to a complex clinical situation was deduced as per the ayurvedic fundamentals and it was found that the treatment principles through which the patient was treated were essentially the same as are depicted in ayurveda.
A Hindu male of about 41 year age reported to Vatsala Hospital, Lucknow with severe pain and distention in abdomen for 1 day. On examination he was found to have severe tenderness on the right side of the abdomen increasing more by lying on the side. He was reported to have loose stools for one day but had a history of severe constipation otherwise. He was unable to eat anything since last three days due to pain and distention in abdomen. He was looking pale, prostrated and agonized. Further history revealed him having fever for past 6 months and having poorly controlled diabetes since 4 years. He reported to have lost weight significantly in past six months.
On further examination he was found to have severe dehydration, dry and coated tongue, loose and flabby muscle mass especially at calf region, lowered blood pressure and rapid pulse. The temperature was slightly elevated.
The patient was immediately investigated for his routine blood counts and blood sugar. A sonographic examination of the abdomen along with an X-ray abdomen in erect posture was also done in order to reveal any abdominal pathology.
Sonographic finding revealed a distention in abdomen with multiple mesenteric lymph nodes in abdomen, hepatomegally and an inflammatory or otherwise thickened structure in the bowel at right ilio cecal junction extending to cecum. Blood count had shown a pronounced leucocytosis with predominance of neutrophils. Random blood sugar was found elevated.
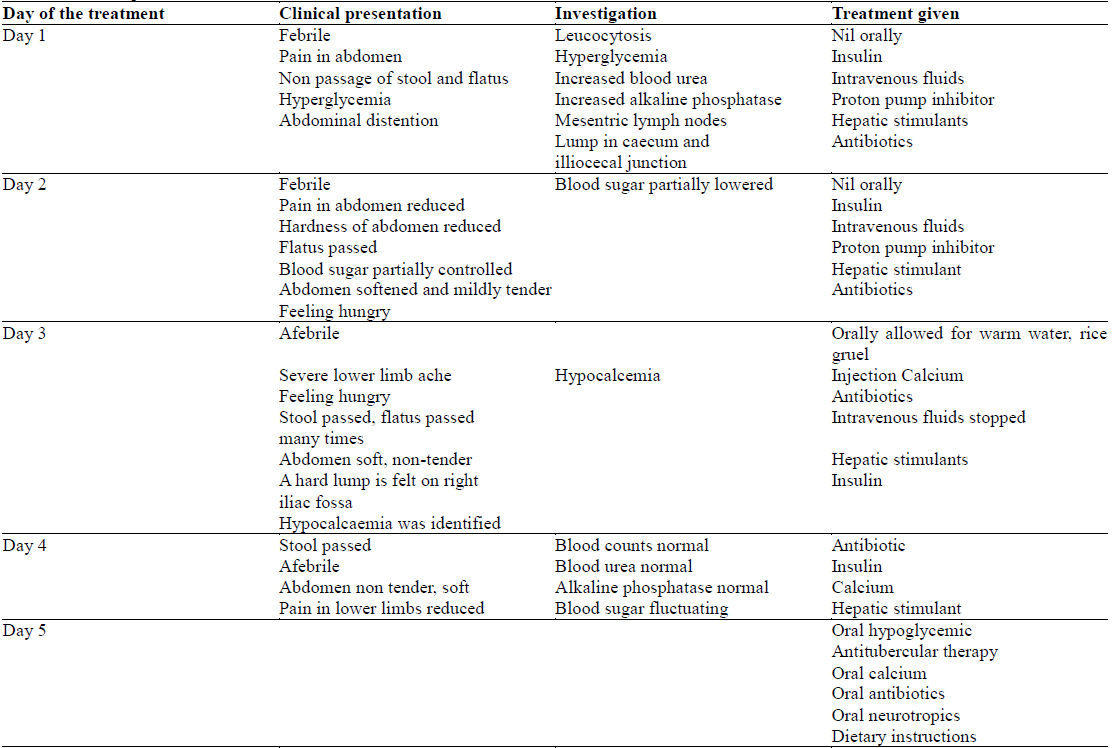
eutrophils. Random blood sugar was found elevated. With this clinical and investigational picture the patient was diagnosed as having sub-acute intestinal obstruction with un controlled Diabetes. He was given following treatment (Table 1):
[Table 1.] Clinical presentation and the treatment recommended
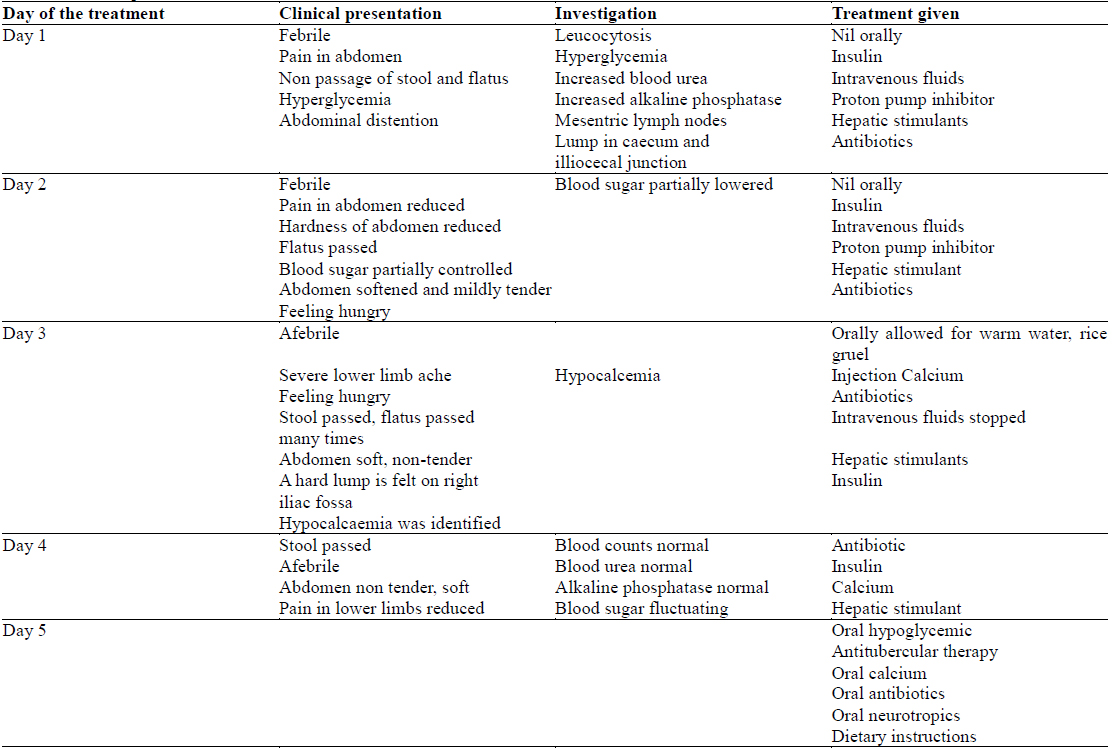
Clinical presentation and the treatment recommended
With these instructions on day 5 the patient was advised to continue the given medicine for 15 days and then to come for a follow up
Now at this stage when the patient is still improving, this would be much interesting to see if this treatment protocol which seem to have been tailored as per the modern understanding of the disease, has something common with ayurveda. We therefore deduced the case as per the ayurvedic understanding and discussed its management as per ayurveda and then subsequently we tried to identify the commonalities of principles in modern medicine and ayurveda.
>
Ayurvedic understanding of the case
The patient was apparently having a pitta-vata dominant prakriti (a fire and air dominant constitution) which was visible through his physical appearance. The dushti (pathogenesis) involved mainly of kapha (water) and vata (air) and the ashraya (place) of the dushti was maha srotasa (gastrointestinal tract). A pronounced agnimandhya (reduced digestive fire) was observed and eventually the features of koshtha gata ama (gastrointestinal indigestion) and dhatu gata ama (improper processing of nutrients at cellular level) were visible. The features representing agnimandhya, amajirna (indigestion) and vishtabdha jirna (distended abdomen due to indigestion). The predominant feature were sharir Gaurav (heavy ness of the body), Utklesha (nausea), Gandakshi kuta Shotha (edema around eyes and face) pertaining to amajirna; shula(pain), adhman (distension), toda (piercing pain), bheda (cutting pain) (abdominal pain of various presentation), mala adho vayu apravritti (absence of flatus and stool), stabdhata (rigidity), anga peedan (body ache) pertaining to vistabdha jirna. With this initial presentation patient required an ama pachan (digestion of undigested substances) intervention initially followed by a treatment strategy to handle the cause of recurrent ama (undigested material) production. Langhan (fasting) was initially prescribed as modality to induce amapachan. After two complete day of langhana when the ama level reduced and clinical signs showing the improvement in agni (digestive fire) status (noted through passage of flatus, softened abdomen), the patient was allowed to have warm water which further helped in ama pachana (Rastogi, 2010).
Subsequent to this initial treatment, agnimandhya and ama was found to be caused by an apparent infection causing chronic fever visible through the leucocytosis. As a vyadhipratyanika (focusing upon disease) approach to deal with the cause of the fever, an antibiotic may be given which could have countered the cause of the fever and subsequently could have relived the features of the ama and agnimandhya. With this treatment approach, the fever subsided and also the features of ama and as a result the appetite improved, flatus and stool passed and abdomen softened (Singh, 2014).
Subsequently the patient was noticed for having a pronounced dhatu kshaya (emaciation) predominantly mamsa (muscles), meda (fat) and asthi (bone). It was visible clinically in the form of regular loss of weight, reduced muscle tone particularly to the calf muscle area, reduced muscle bulk and loss of subcutaneous fat. The patient reported to have severe bone pain in lower limbs from second day of his treatment. An investigation for serum calcium was found substantially low. Long bones for being ashraya place of vata are having larger possibility of representing the features of vata dushti (abnormality of air). The patient was identified to have vata dominant prameha (diabetes) leading to dhatu kshaya and vata prakopa causing pain in lower limbs. As a vyadhi pratyanika approach again, the patient was given adequate dose of insulin to balance vata by providing nutrition to tissues and cells. At the same time vataashraya in long bones was also supplemented with calcium which could have added to the treatment of asthikshaya (loss of calcium from bones) and the pain which was caused by the vata dushti. For the purpose of agnideepan (stimulation of digestive fire) and vatanulomana (improved peristalsis), additionally some hepatic stimulants were also given. These have resulted in agni improvement and also the improved peristalsis which might have added to the softening of abdomen, passage of flatus and stool (Patwardhan, 2014).
This treatment has resulted in substantial improvement in clinical picture of the patient. This is much surprising to see the similarity of the ayurvedic treatment principles with that of modern medicine. When seen in light of modern science, we hardly find any reason of disapproving ayurvedic treatment approach in this case deduced as per the principles of the modern science (Lakhotia, 2013).
By observing through this case we may find a homology of various treatment approaches between these two apparently distinct health care sciences.
Ayurveda and modern health care seem to have different rooting and different treatment approaches based upon their own dogma of disease and its cure. Interestingly, in a cross sectional view, many treatment approaches of ayurveda look similar to what modern medicine thinks of in a particular condition and many such modern approaches can also be beautifully deduced as per the ayurvedic principles. The idea of this discussion is to identify the commonalities and homologies of ayurveda and modern medicine and to see that the differences which may appear between these two streams of health care science are more artifacts rather than of being realistic in nature. A tolerant view point towards both of these systems therefore can be a wonderful way of synthesizing the best medicine by due incorporation of modern science along with the ancient wisdom, a thought which requires to be nurtured for a larger cause of humanity.
By seeing this case, we can easily deduce that there are no reasons of considering a system untouchable when it really follows almost same kind of principles although with a different nomenclature and different way of interpretation but essentially reaching to the same ultimate goal as the other stream is going. It’s like different streams of water ultimately aiming to converge at sea carrying the different qualities in the water as per the soil they are passing through.
Another important lesson which can be learnt from this case is to adopt a counter approach of research in ayurveda. Since long ayurveda is solely relying upon its material resources which are recommended in its ancient classics. There had been insignificant approaches to incorporate new components in ayurveda to enrich it as per the contemporary needs and also to enrich its resources. Till now ayurveda and its research is busy proving its effects in terms of modern biology. Every ayurvedic treatment is being tried to be evaluated critically on the basis of established modern biological facts. This is good that it endorses the principles and practices of ayurveda in terms of modern science. But at the same time, there is also an urgent need of testing the things from realm outside ayurveda to see if they can be incorporated in ayurveda for its further enrichment.
Seeking the ayurvedic analysis for modern principles of treatment and investigations can be one important way of enriching ayurveda through the science which is already known and is in practice. For example, in fever, the features of ama are very apparent. Now any treatment approach which counters the fever, would eventually lead towards the normalization of ama features and hence can be called as an amapachaka in ayurvedic terminology. An analgesic which reduces pain would be a vata shamak, an anti-inflammatory which reduces swelling and pain would be a pitta shamak in a similar tone. Prokinetics which improve the gastrointestinal movements can well be termed as vatanulomaka and hepatic stimulants which improve the appetite may be the deepana (digestive stimulants) and pachana (digestents) drugs for similar reasons. A huge sum of inference can be made like this to enrich ayurveda for more of the drugs which are tested and are in use for a variety of clinical conditions.
We would soon be landing on the conclusion that none of the material existing on the earth can be denied of having a medicinal property provided if it is used properly, a dogma which was promoted by ayurveda centuries ago.