The aim of this study was to examine whether there is an association between vitamin intakes and established periodontitis in Korean adult population. The 6,245 subjects aged over 19 years old, who participated in health survey, oral examination and nutrition survey were selected for this study from the database of the Fourth Korean National Health and Nutrition Examination Survey. Established periodontitis was defined as ≥ code 3 in community periodontal index. Vitamin intake was assessed with the food-frequency questionnaire. In analysis, participants were classified by quintile of vitamin intakes. We also considered covariates as socio-demographic characteristics, health-related behaviors including physical activities, systemic diseases and oral health-related behaviors. Multiple logistic regression was performed to assess the crude and adjusted associations. All analyses considered a complex sampling design using SAS 9.2. In crude analysis, less intake of vitamin A, retinol and vitamin B2 significantly increased the risk of periodontitis (vitamin A, odds ratio [OR] Q1=1.00, Q2=0.73, Q3=0.80, Q4=0.77, Q5=0.78; retinol, OR: Q1=1.00, Q2=0.86, Q3=0.73, Q4=0.62, Q5=0.55; vitamin B2, OR: Q1=1.00, Q2=0.70, Q3=0.63, Q4=0.67, Q5=0.68). However, after adjusting for socio-demographics, general and oral health status and behaviors, only vitamin B2 was significantly associated with established periodontitis (OR: Q1=1.00, Q2=0.72, Q3=0.73, Q4=0.76, Q5=0.84). An adequate vitamin B2 intake was significantly associated with a decreased risk of periodontitis. This finding shows that nutrient intake is slightly correlated with periodontitis in Korean adult population. Further studies are needed to understand this association between nutrients intake and periodontitis in more details.
본 연구는 국민건강영양조사 제4기 자료를 이용하여 한국 성인에서 비타민 섭취와 치주염과의 관련성을 구명하고자 하였다. 국민건강영양조사 원시자료에서 건강조사와 구강검진 및 식이조사에 모두 참여한 19세 이상 성인 6,245명의 자료를 추출한 후 복합표본설계를 반영하기 위하여 가중치를 고려한 통계분석을 실시하였다. 대상자의 인구사회학적 특성, 전신건강상태와 행태, 구강건강상태와 행태 및 비타민 섭취 5분위에 따른 치주염 유병률의 차이를
Periodontitis is a major oral health problem, which affects a considerable proportion of the adult population. Li et al.1) explained that periodontitis is disorders of the gums, gingival, and other tissues around the teeth. Moreover, periodontitis is the most common chronic inflammatory disease involving gingival inflammation and the destruction of periodontal tissue2-4).
Nowadays, inflammatory periodontitis affects 10 to 15 percents of the world’s population and is a major cause of tooth loss in adults5). An estimated 8% to 10% of American adults have some form of periodontitis, on the other hand, Kwon et al.6) reported that the prevalence of periodontitis is 73.4% among aging over 19 years old in Korea. By the reduced prevalence of caries and subsequent loss of teeth in the aging population, periodontitis has become a more significant problem7).
Stewart et al.8) reported that oral health is an essential component of health throughout life and is recognized to be an important determinant of nutritional status and general health. Thus, poor oral health status is associated with poor nutritional health, just as inadequate nutrition can affect oral health9). Nutritional factors have been implicated in several chronic inflammatory diseases as risk factors included oral health such as periodontitis10). A few studies reported that there were more associations between nutrition and periodontitis as an inflammatory disease, including the effect of vitamin C, vitamin E, and carotenoids as dietary antioxidants in inflammation modulation11), and the impact of obesity on modulating the host’s immune and inflammatory system leaving the patient with a greater risk of periodontitis12). Eating habits and nutrients also influence periodontitis, some studies also have reported that consumption of vitamin C, E and calcium is connected to periodontitis13).
Vitamin is the one of nutrients associated with periodontits. In particular, vitamin C is also an effective nutrient in treatment of acute necrotizing ulcerative gingivitis (ANUG)14). Melnick et al.15) reported ANUG has provided the evidence for an association between ascorbate deficiency and disease risk. Furthermore, there is biological plausibility for such an association between vitamins and periodontitis, due to the role of ascorbate in collagen synthesis and leukocyte function. According to the most studies relating nutrition and oral health, vitamin A and iron improve host resistance to infections, vitamin C, D, E reduce tissue destruction and enhance wound healing, and vitamin D and calcium also have a beneficial effect on bones and tooth retention16). Moreover vitamin C deficiency is known to reduce the host immune response by increasing the activity of polymorphonuclear leukocytes17). For these reasons, a well-balanced diet and vitamin intakes should be required for maintenance of optimal general and oral health18).
Studies related to the association between diet and established periodontitis are sufficient; however, analytical study about the association between vitamin intake and established periodontitis is still inadequate. This study is hypothesized that vitamin intake is directly associated with periodontitis.
The aim of this cross sectional study is to examine whether vitamin intake is independently associated with established periodontitis adjusted for socio-demographic characteristics, general and oral health status, and those related behaviors using a representative sample of Korean adults.
The data of this study was a subset of the Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV) which was conducted in 200919). The total of 7,893 subjects over 19 years old were selected from the database of the KNHANES IV. Among of them, only 6,245 subjects, who participated in health survey, oral examination and nutrition survey, were included in this study.
1) Periodontitis
Periodontitis was assessed by community periodontal index (CPI) based on bleeding, presence of calculus, and pocket depth at sextant of mouth. The CPI score was rated into 5 categories at each sextant: sound (CPI 0), gingival bleeding (CPI 1), calculus (CPI 2), shallow periodontal pocket of 3.5∼5.5 mm (CPI 3), and deep periodontal pocket of 5.5 mm or more (CPI 4). In this study, the subject’s CPI score was recorded the highest score of the sextant. According to the subject’s CPI score, established periodontitis was defined as the highest CPI score of sextant ≥code 320).
2) Vitamin intakes
The food-frequency questionnaire was designed to estimate daily amount of food-group consumption and nutrient intake the day before the survey started (24-hours recall method). The trained nutritionists visited individual participants in each household to interview about diet and meal patterns of the 97 food items. The consumption of a food item was estimated by multiplying the standard portion size by its intake frequency. Vitamin intakes were calculated based on the standard food composition table in Korea19).
In this study, the 5 kinds of vitamins were evaluated such as vitamin A, retinol, vitamin B1, vitamin B2, and vitamin C and then classified by quintiles of amount of intakes: Q1 (intake≤1st quintile), Q2 (1st quintile<intake≤2nd quintile), Q3 (2nd quintile<intake≤3rd quintile), Q4 (3rd quintile<intake≤4th quintile), and Q5 (4th quintile<intake).
3) Covariates
The socio-demographic characteristics, general health status and related behaviors, and oral health status and related behaviors were considered as covariates in this study. The socio-demographic characteristics included gender, age, marital status, education level, and income. Income was classified by quartiles of monthly household income investigated in Korea Centers for Disease Control and Prevention19) (2010): low (<25%), middle-low (25∼50%), middle-high (50∼75%), and high (>75%).
The general health status and related behaviors included perceived health status, cardiovascular disease (CVD), diabetes mellitus (DM), body mass index (BMI), alcohol consumption, smoking status, and physical activity. Scores from the alcohol use disorder identification test with four categories classified the alcohol consumption: normal (0∼8), hazardous (9∼12), dependence (13∼19), or harmful (more than 20).
The oral health status and related behaviors included the number of decayed, missing, or filled tooth, perceived oral health status, daily frequency of tooth-brushing, experience of dental checkup in the past 1 year, and use of dental auxiliary device.
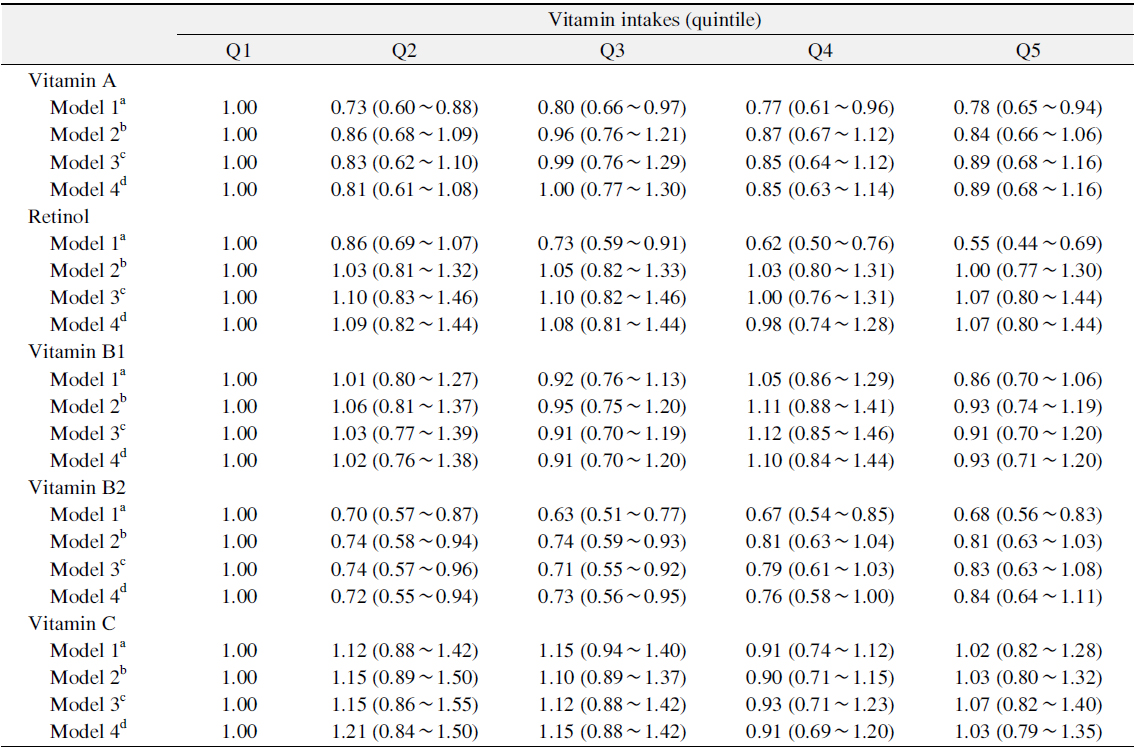
The prevalence of periodontitis according to the socio-demographic characteristics, general health status and related behaviors, oral health status and related behaviors, and quintiles of vitamin intake was summarized by weighed percent and 95% confidence interval (CI), and then analysed by chi-square test procedure accounting for individual weight of complex sampling design. To access the crude or adjusted associations between vitamin intakes and periodontitis, odds ratio (OR) and 95% CI were calculated by multivariate logistic regression model. Four models were fitted to assess an association between vitamin intakes and established periodontitis. Model 1 was a crude association between vitamin intakes and periodontitis. Model 2 was an association between vitamin intakes and periodontitis after adjusting for socio-demographic characteristics. Model 3 was an association between vitamin intakes and periodontitis after adjusting for sociodemographic characteristics and general health status and related behaviors, and model 4 was an association between vitamin intakes and periodontitis after adjusting for socio-demographic characteristics, general health status and related behaviors, and oral health status and related behaviors.
Statistical analyses were conducted by SAS 9.2 for Windows (SAS Institute Inc., Cary, NC, USA), and considered statistically significant as a p-value of <0.05.
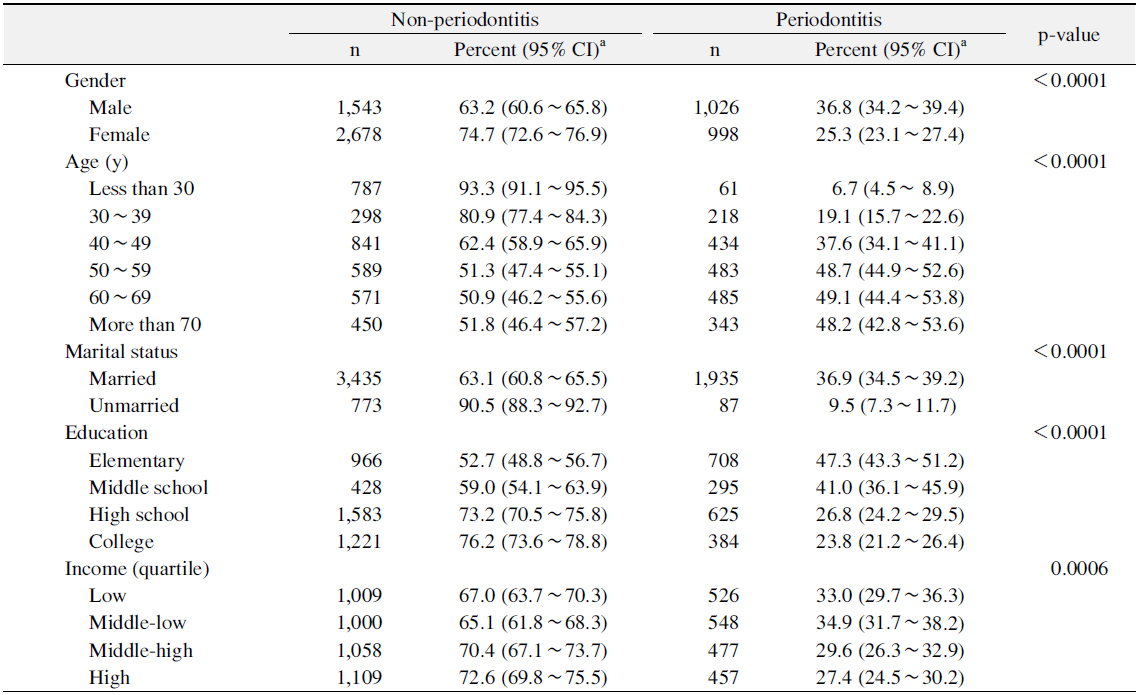
Table 1 showed the prevalence of periodontitis according to the socio-demographic characteristics. The prevalence of periodontitis was significantly higher for males, married persons, and persons aged over 50 years than for females, married persons, and those in other age groups (p<0.05). The prevalence of periodontitis was significantly lower for graduated high school or above and more than middle-high income levels than for those in other education and income groups (p<0.05).
[Table 1.] Prevalence of Periodontitis according to Socio-Demographic Characteristics
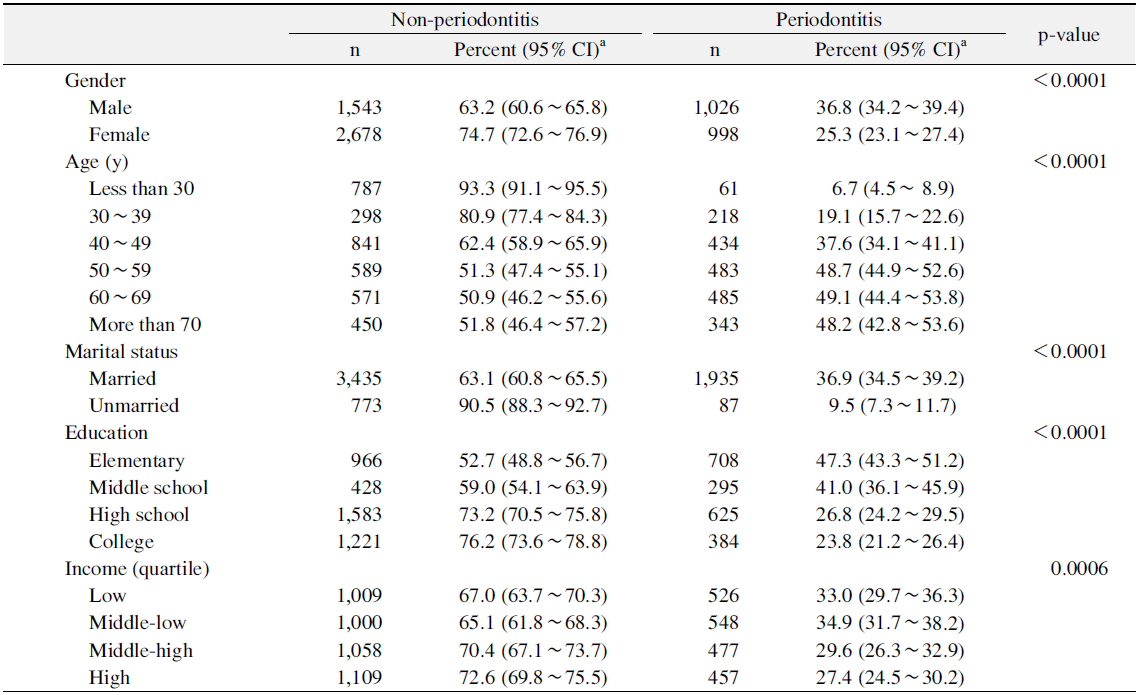
Prevalence of Periodontitis according to Socio-Demographic Characteristics
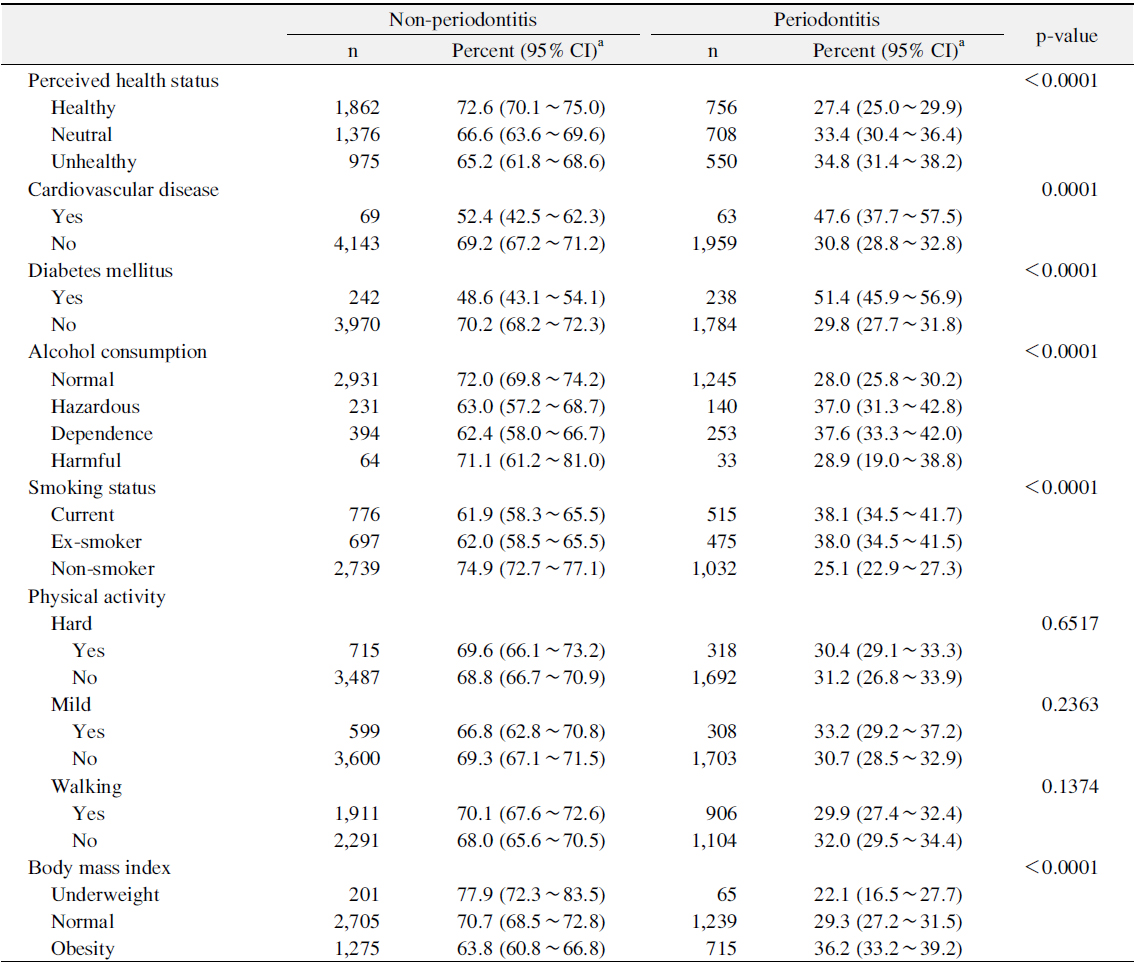
Table 2 showed prevalence of periodontitis according to the general health status and related behaviors. The prevalence of periodontitis was the lowest for persons who answered ‘healthy’ in perceived health status (p<0.05). The prevalence of periodontitis was significantly higher for persons with CVD or DM than for those without CVD or DM (p<0.05). The prevalence of periodontitis was significantly lower for normal alcohol consumption and non-smoker groups than for those in other alcohol consumption and smoking status groups (p<0.05). Moreover, the prevalence of periodontitis was significantly higher for obesity group than for those in other BMI groups (p<0.05).
[Table 2.] Prevalence of Periodontitis according to General Health Status and Related Behaviors
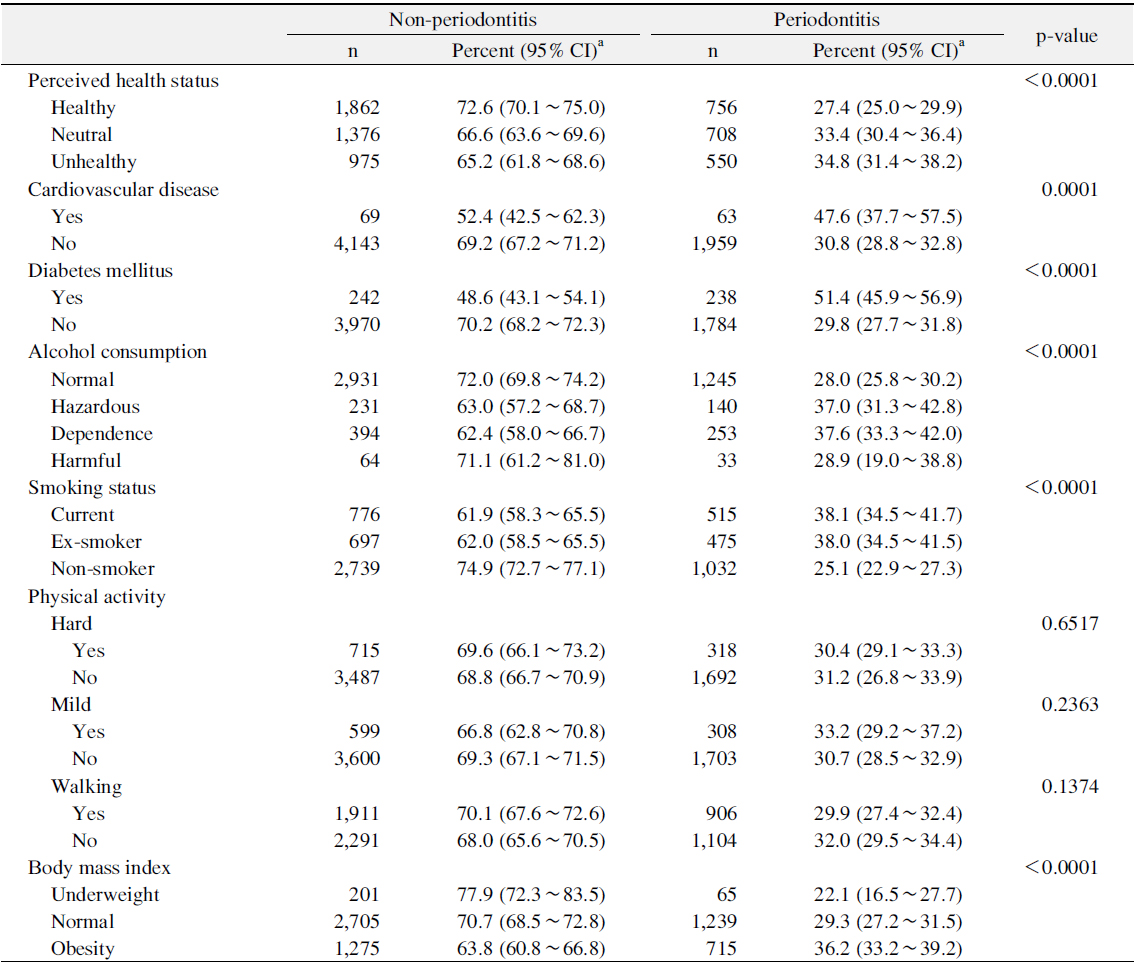
Prevalence of Periodontitis according to General Health Status and Related Behaviors
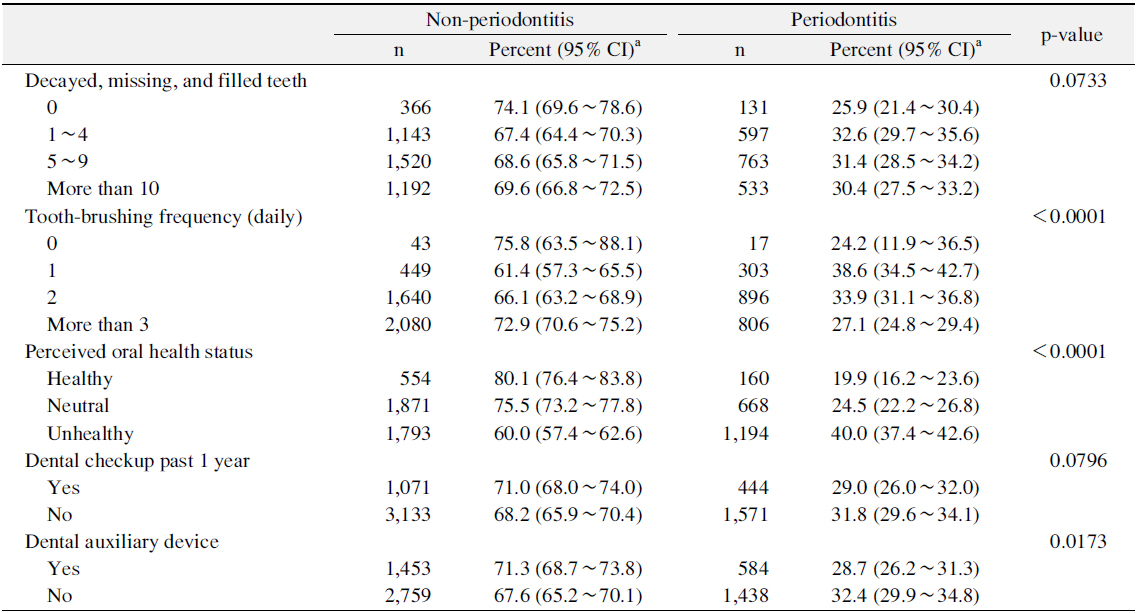
Table 3 showed prevalence of periodontitis according to the oral health status and related behaviors. The prevalence of periodontitis statistically decreased with increasing toothbrushing frequencies (p<0.05). The prevalence of periodontitis was the highest for persons who answered ʻunhealthyʼ in perceived oral health status (p<0.05). Moreover the prevalence of periodontitis was significantly lower for persons used dental auxiliary device than for those not used dental auxiliary device (p<0.05).
[Table 3.] Prevalence of Periodontitis according to Oral Health Status and Related Behaviors
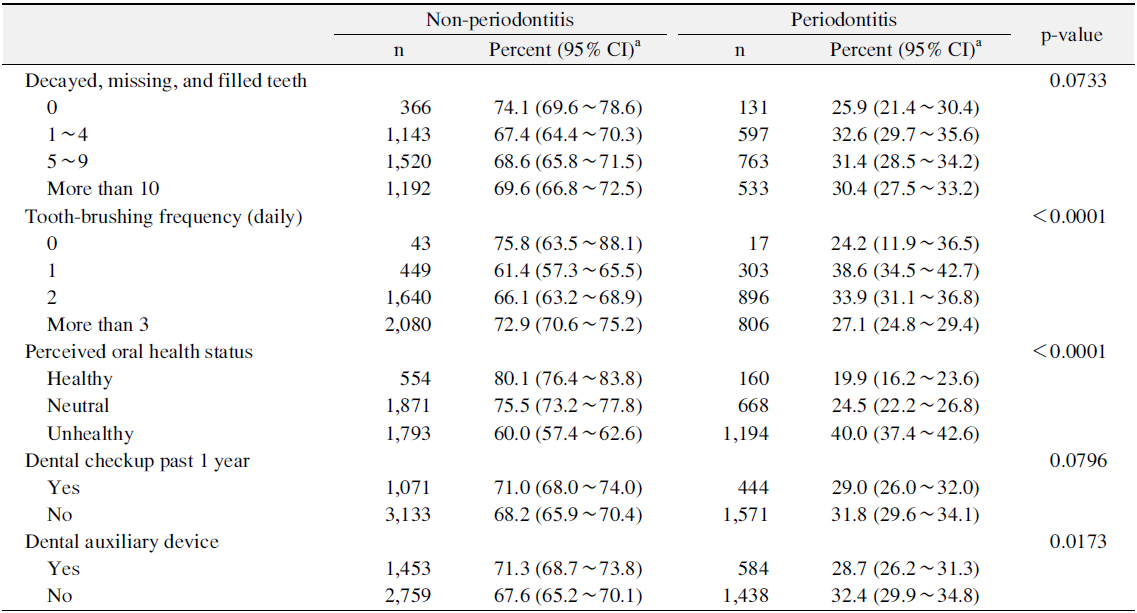
Prevalence of Periodontitis according to Oral Health Status and Related Behaviors
Table 4 showed the association between vitamin intakes and established periodontitis. The persons who had a fewer intakes of vitamin A, retinol and vitamin B2 had a greater risk of periodontitis (vitamin A, OR: Q1=1.00, Q2=0.73, Q3=0.80, Q4=0.77, Q5=0.78; retinol, OR: Q1=1.00, Q2=0.86, Q3=0.73, Q4=0.62, Q5=0.55; vitamin B2, OR: Q1=1.00, Q2=0.70, Q3=0.63, Q4=0.67, Q5=0.68). Moreover, after adjusting for all confounding variables, only vitamin B2 was significantly associated with established periodontitis (OR: Q1=1.00, Q2=0.72, Q3=0.73, Q4=0.76, Q5=0.84). However, vitamin B1 and vitamin C were not significantly associated with established periodontitis in crude and adjusted analysis.
[Table 4.] Association between Vitamin Intakes and Established Periodontitis
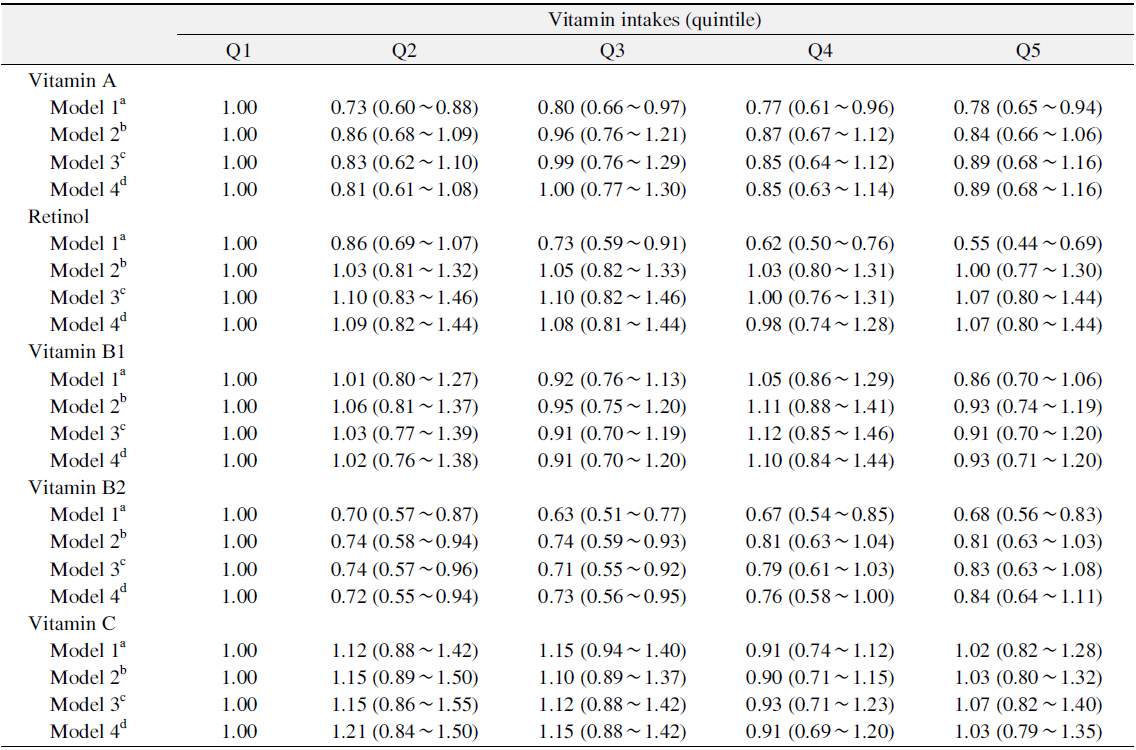
Association between Vitamin Intakes and Established Periodontitis
This study investigated the association between vitamin intake and periodontitis using the data from the KNHANES IV.
In this cross sectional study, there was not consistently significant association between vitamin intakes and periodontitis in Korean adult population. However, after adjusting for confounding variables, only vitamin B2 was significantly associated with established periodontitis. Our findings supported that vitamin B2 deficiency was associated with periodontitis. Neiva et al.21) demonstrated that vitamin B complex could positively influence wound healing processes. Vitamin B complex supplement in combination with access flap surgery resulted in statistically significant superior clinical attachment levels gains. Vitamin B2, also called riboflavin, is one of eight vitamin Bs. Most healthy people who eat a well-balanced diet get enough riboflavin. However, elderly people and alcoholics may be at risk for riboflavin deficiency because of poor diet. Symptoms of riboflavin deficiency include fatigue, slowed growth, digestive problems, cracks and sores around the corners of the mouth, swollen magenta-colored tongue, eye tiredness, swelling and soreness of the throat, and sensitivity to light.
In previous study, vitamin C was significantly associated with periodontal disease. Paek and Lee22) reported vitamin C intake is significantly associated with periodontitis in Korean adults, and also suggested that vitamin C will be helpful in the prevention of periodontitis. Nishida et al.23) found a relationship between reduced dietary vitamin C and increased risk for periodontal disease for the representative of the US population. Meanwhile, although in some studies decreased dietary vitamin C intake was found to be associated with increased risk of periodontal disease, no conclusive evidence could be demonstrated24). Our results showed that periodontitis was not clearly associated with vitamin C. A possible clarification is that serum levels reflect only the present nutritional status and not the lifelong times past. Furthermore, serum levels are affected by several factors, for example recent dietary intake, diurnal variability, concomitant medication, inflammations, and stress25).
Stein et al.26) reported vitamin D is also potential role in protecting the periodontium as well as in regulating periodontal wound healing. On the other hand, Lee and Roh27) reported vitamin D has a significant negative correlation to periodontal disease among the post-menopausal women including the women who underwent bilateral ovariectomy. This study could not determine any association between vitamin D and periodontitis due to lack of data. This association must be confirmed in future.
Bawadi et al.12) found that a low physical activity level and a poor diet were significantly associated with increased odds of periodontitis throughout conducting to determine the relationship between physical activity, healthy eating habits and periodontal health status among adults in Jordan. However, our findings showed that physical activity even divided into hard and mild physical activity and walking was no statistically significant difference in the prevalence of periodontitis. Further study will be need to study about why the reason the current study was not significant difference of the association physical activity and periodontitis in great detail.
There were a few limitations even though the study showed that vitamin intakes were significantly associated with established periodontitis in the Korean adult population. The CPI assessed the periodontal status. Although CPI is an easier way of evaluating the periodontal treatment needs in a community setting, it can overestimate or underestimate the prevalence of periodontitis because the use of representative teeth includes pseudo pockets. One of the most important limitations of this study is its cross-sectional study design, which makes it impossible to determine the direction of the causal relationship between vitamin intakes and periodontitis. Therefore, this study was to assess the independent association of vitamin intake and periodontitis for adjusting an influence of possible confounded variables such as socio-demographic characteristics, general health behaviors and status, and oral health behaviors and status.
This study was conducted comprehensively in the Korean representative population sample. Vitamin B2 was just considerably associated with established periodontitis. An adequate vitamin B2 intake was significantly associated with a decreased risk of periodontitis. Past studies about the association of vitamin intakes and established periodontitis is still sufficient, however, this finding shows that vitamin B2 intake is correlated with periodontitis. Prospective studies are required to identify the link between vitamin intakes and periodontitis from longitudinal database. Furthermore, the underlying biological mechanism presentation a causal effect relationship between vitamin intakes and established periodontitis remain to be found out through prospective cohort studies.