The purpose of this study is to investigate the research about using tuina therapy for depression and to determine its efficacy.
All relevant articles were searched in the China National Knowledge Infrastructure using the terms ‘tuina’ and ‘depression’.
Forty-one studies were selected, 34 randomized controlled trials (RCTs) and 7 prospective studies. The Chinese Classification of Mental Disorders and Hamilton Depression Rating Scale were used most frequently as diagnostic criteria and an assessment tool, respectively. Conduction exercise therapy was used in all studies; in contrast, Zheng Xing exercise therapy was used in only 1 study of depression patients with neck vertebrae disease. In 9 RCTs that showed scores of more than 2 points on a modified Jadad scale, tuina therapy had significant antidepressant efficacy compared with conventional treatment. However, more high-quality studies are required.
Tuina therapy has a valid therapeutic effect on depression according to studies published in China; if evidence accumulates from high-quality studies, it can be considered a non-pharmacologic treatment for depression in Korean medicine, as well.
Massage therapy, so-called ‘tuina’ (推拿), is one of the therapeutic technique in Traditional Chinese Medicine (TCM) to treat and prevent diseases, by rubbing, kneading, or percussion of the soft tissues and joints of the body with the hands, usually performed by one person on another, esp. to relieve tension or pain1). In general, tuina therapy which is a typical manipulative therapy in TCM has been used for musculoskeletal disorders, pain disorders, body modification, and rehabilitation. And its application range is expanding increasingly. Globally manipulation is used to improve various medical system diseases such as eye disease, cardiovascular disease, and otolaryngology disease as well as musculoskeletal disorders and pain disorders2). Also manipulation therapy is even used for psychiatric disorders like anxiety3), depression4), and insomnia5) to treat or relief their symptoms.
Among them, depression which is one of the major psychiatric disorders generally known to use antidepressants like selective serotonin reuptake inhibitor (SSRI), but because of considerable side effects and its limits of treatment, nonpharmacological treatments are often used as complementary6). Nonpharmacological treatment is not only applicable effectively to a patient refusing drug treatment, but also known to have synergistic effect when it used with medication7). Therefore its importance in the clinical field could be considered high.
In TCM, since ancient times, nonpharmacological treatments such as acupuncture, moxibustion, cupping, and massage therapy has been applied to treat various diseases as well as traditional herb medicine. They are not just simple treatment technique, and has been used as object-oriented treatments according to the state of patient’s condition and neuropathy based on the theory of TCM. Thus in depression, which is important to care with nonpharmacological intervention, traditional nonpharmacological treatment can be used more efficiently by providing a comprehensive care according to the condition of patient as well as state of the disease.
Until now, depressive effect of acupuncture8) and moxibustion9) has been reported in Korea, but there is no research about the impact of tuina therapy on depression yet. In this study, we are purposed to investigate trend of the researches and to identify the effectiveness of tuina on depression by searching relevant articles through the Chinese database ‘China National Knowledge Infrastructure (CNKI)’. And it expected to be used in the progress of developing clinical guidelines related with depression as a data for determine the effectiveness of tuina therapy and as a reference for design of clinical research.
Studies included in this review were clinical trials or prospective studies that examined participants with depression using tuina therapy. Studies that not associated with depression, review articles, and not specified diagnostic criteria or screening tool in inclusion criteria were excluded. In order to identify the effects of tuina therapy, studies using same massage intervention for treatment group and control group were excluded. Intradermal acupuncture, acupoint sticking therapy, self-acupressure, and manipulation which is not applied theory of TCM were considered to be not included in tuina therapy. Master’s thesis and doctoral thesis were included.
Chinese database (CNKI, 中國知識基礎施設工程) were searched until up July 2015, using terms ‘tuina’ and ‘depression’ (‘忧郁 OR 抑郁’ [主题] AND ‘推拿’ [主题], ‘忧郁 OR 抑郁’ [主题] AND ‘按摩’ [主题], ‘忧郁 OR 抑郁’ [主题] AND ‘导引’ [主题], ‘depression’ [subject] AND ‘tuina’ OR ‘massage’ [subject])
In order to evaluate the quality of the study design, we used modified Jadad scale to assess RCTs. Modified Jadad scale is a modification of the existing evaluation methods of Jadad scale to reflect the difficulty of setting study design, especially blind study, in Traditional Chinese Medicine10). In this study, according to the modified Jadad scale, we graded scores in the following order:
1) 1 point was added if research was conducted randomly assigned (randomization) 2) 1 point was added if the randomization method is described and appropriate 3) 1 point was added if research was conducted as subject blinded 4) 1 point was added if research was conducted as evaluator blinded 5) 1 point was added if withdrawals and dropouts are described
4. Classification of Tuina therapy
In accordance with the method and purpose, tuina therapy has a very broad and individual features. To investigate the effect of tuina therapy more in detail, we classified tuina into two ways11).
1) Conduction exercise (導引推拿)
Tuina therapy to control qi (氣) and blood (血) by the application of hand techniques to the patient’s skin surface, meridians and acupoints.
2) Zheng Xing exercise (正形推拿)
Tuina therapy to improve the activity by stretching the meridian sinew (經筋推拿) or to restore the dislocation or fracture by using orthodontic techniques to the anatomical imbalance (整骨推拿).
We classified tuina of simple physical stimulus on surface of the skin, meridians or acupoints as conduction exercise on the other hand massage of orthodontic therapy on muscles or skeleton to correct the local tensions or deviation as Zheng Xing exercise.
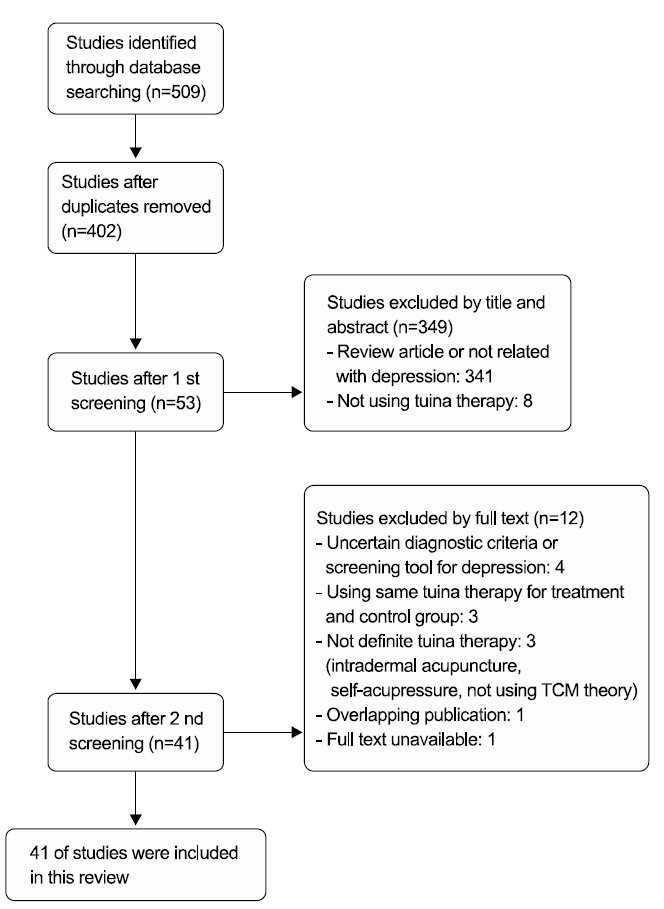
Total 509 studies were screened and 107 duplicated studies were excluded. 341 studies not related with depression or review articles, and 8 studies not related with tuina therapy were excluded by title and abstract screening. After 1st screening, by full text screening, 4 studies not describing certain diagnostic criteria or screening tool for depression, 3 studies using same tuina therapy for treatment and control group, 3 studies not using definite tuina therapy (intradermal acupuncture, self-acupressure, and not using TCM theory), 1 studies overlapping publication, and 1 studies unavailable to get full text. Lastly 41 studies were remained and examined tuina therapy for depression (Fig. 1).
The 41 studies included conclusively in this review contain 34 RCTs (82.93%), and 7 prospective studies (17.07%). In RCTs, there were 5 master’s thesis.
1) Classification by research topic
According to the content of diseases type, they were divided into 2 categories, studies of depression alone and studies of depression comorbid with other conditions. The former include 11 RCTs, and 2 prospective studies while the latter include 23 RCTs and 5 prospective studies.
2) Subject
In case of 23 RCTs of depression comorbid with other conditions, post stroke depression was the most frequent subject as 7 pieces (30.43%), and 6 pieces (21.74%) about postpartum depression followed. And in 5 prospective studies, postpartum depression was the most frequent subject as 3 pieces (60.00%).
Throughout the studies included in this review, there were 7 studies (17.07%) using pattern identification as a screening tool.
3) Diagnostic criteria/Screening tool
Of the total 41 studies, studies describing depressive disorder diagnostic criteria were 32 pieces (78.05%). Among them Chinese Classification of Mental Disorders (CCMD) was the most commonly used as 16 pieces (68.75%), Diagnostic and Statistical Manual of Mental Disorders (DSM) as 4 pieces (12.50%), and International Classification of Disease (ICD) as 3 pieces (9.38%) followed.
Of the total 41 studies, studies describing depressive disorder screening tool were 24 pieces (57.14%). Among them Hamilton Depression Rating Scale (HAMD) was the most commonly used as 15 pieces (62.50%), and Self-Rating Depression Scale (SDS) as 5 pieces (20.83%) followed.
Other than, in case of senile depression or postpartum depression, Geriatric Depression Scale (GDS) or Edinburgh Postnatal Depression Scale (EPDS) were used respectively.
4) Assessment tool
Of the total 41 studies, most of studies (95.12%) describing the assessment tool except for 2 prospective study. Among them, for depression symptom, HAMD was the most commonly used as 27 pieces (69.23%), SDS as 11 pieces (28.21%), and EPDS as 5 pieces (12.82%) followed. For other symptoms, Pittsburgh Sleep Quality Index (PSQI) was the most commonly used as 5 pieces (12.82%).
Other than, in case of depression with diabetes or postpartum depression, fasting blood glucose (FBG) and glycated hemoglobin (HbA1c) or estradiol (E2) and follicle stimulating hormone (FSH) were used respectively
5) Treatment period
Of the total 41 studies, most of studies (97.56%) described the treatment period except for 1 prospective studies. Among them, the period of ‘more than 4 weeks, under 8 weeks’ was the most commonly used as 24 pieces (60.00%), ‘more than 8 weeks, under 12 weeks’ as 9 pieces (22.50%), ‘more than 12 weeks’ as 6 pieces (15.00%), and ‘under 4 weeks’ as 1 pieces (2.50%) followed.
6) Intervention
Of the total 41 studies, studies describing the method of tuina therapy were 39 pieces (95.12%), the frequency of tuina therapy were 35 pieces (85.37%), and the total time required to perform tuina therapy at one time were 19 pieces (46.34%).
Among the studies describing the method of tuina therapy, conduction exercise was used in all studies (100.00%), and Zheng Xing exercise was used in only 1 study (2.56%) of depression patients with neck vertebrae disease.
Among the studies describing the frequency of tuina therapy, performing ‘once per day’ was the most commonly used as 25 pieces (71.43%), ‘3 times a week’ or ‘once per 2 days’ as 7 pieces (20.00%) followed.
Among the studies describing the total time required to perform tuina therapy at one time, ‘more than 30 minutes, under 1 hour’ was the most commonly used as 15 pieces (78.95%), ‘under 30 minutes’ as remaining 4 pieces (21.05%) followed.
1) Randomized controlled trial
Of the total 34 RCTs, 33 studies were conducted as a structure of two arm-parallel group, and 1 study as a structure of three-arm parallel group, traditional herbal medicine and tuina therapy for treatment group, traditional herbal medicine or tuina therapy for 2 control group each.
In the 33 two-arm parallel group studies, 24 studies (72.73%) performed common intervention for both group and additional intervention for treatment group. Among them, as a additional intervention, ‘tuina therapy combination with other interventions like acupuncture, traditional herbal medicine, and psychological intervention’ was used as 14 pieces (58.33%), and ‘tuina therapy alone’ as 10 pieces (41.67%).
In the 33 two-arm parallel group studies, 9 studies (27.27%) performed separate intervention for each group without common intervention. Among them, as a intervention for treatment group, ‘tuina therapy combination with other interventions’ was used as 2 pieces (22.22%), and ‘tuina therapy alone’ as 6 pieces (66.67%). And in remaining 1 study (11.11%), ‘tuina therapy alone’ was used for control group, while treatment group received acupuncture intervention.
2) Prospective study
Of the total 7 prospective clinical researches, ‘tuina therapy combination with other interventions’ was used as a intervention.
In order to evaluate the quality of RCTs, modified Jadad scale was performed for 34 RCTs included in this review. Among them, 8 studies using randomized allocation methods on the basis of consultation hours or hospitalization time, 2 studies describing blind with uncertain methods, and 2 studies describing withdrawals and dropouts with poor description did not receive a score.
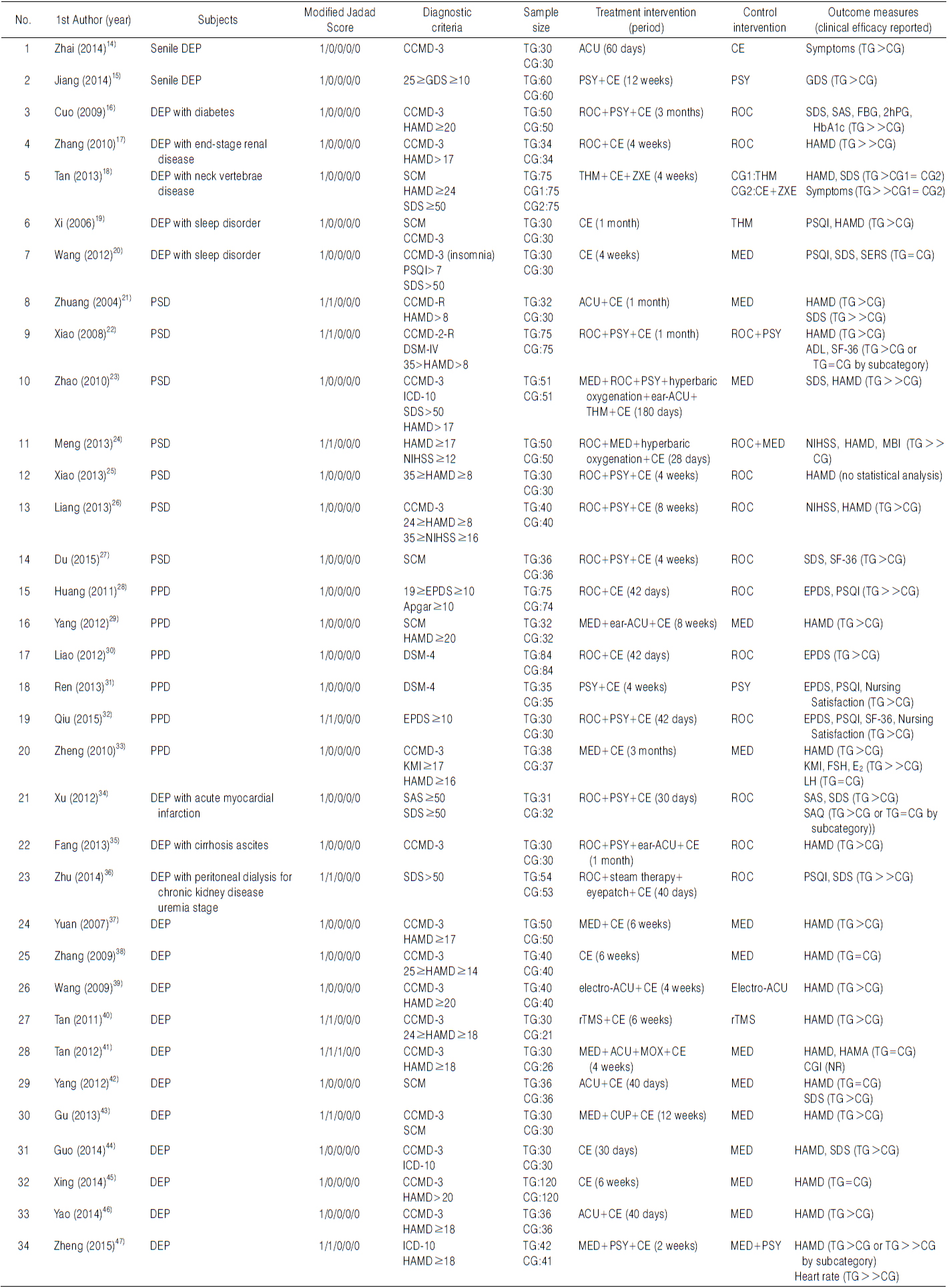
After assessment of RCTs with modified Jadad scale, 25 pieces (73.53%) were for 1 point, 8 pieces (23.53%) were for 2 point, 1 piece (2.94%) was for 3 point, and no piece was for 4 point (Table 1).
[Table 1.] Assessment of RCTs with Modified Jadad Scale

Assessment of RCTs with Modified Jadad Scale
6. Result of study (based on RCTs)
By assessing RCTs scored more than 2 points of modified Jadad scale, 4 RCTs of depression alone, and 5 RCTs of depression comorbid with other conditions were remained.
In case of 4 RCTs of depression alone, HAMD was used in all studies for evaluating therapeutic effect of the intervention. Tan (譚燚飛, 2011) performed repetitive transcranial magnetic stimulator (rTMS) 3 times per week for both group, and additional tuina therapy for treatment group, for 6 weeks to 51 depression patients diagnosed by CCMD, corresponding to 24≥ HAMD≥18, and classified as liver depression and spleen deficiency (肝鬱脾虛). As a result, treatment group was reported to have significantly lower levels of HAMD than control group at 1st, 2nd, 4th, and 6th week after treatment. Also they reported that additional tuina therapy was particularly effective for the initial 1 month. Tan (譚濤, 2012) and Gu (穀建雲, 2013) performed tuina therapy combination with acupuncture, traditional herbal medicine or cupping for treatment group, and drug therapy for control group, respectively for 4 and 12 weeks and to 56 and 60 depression patients diagnosed by CCMD. As a result, treatment group was reported to have significantly lower levels of HAMD than control group. Moreover Tan (譚濤, 2012) reported that in the treatment group compared to the control group, side effects occurred less and lightly based on Treatment Emergent Symptom Scale (TESS). Zheng (鄭碧琴, 2015) performed routine psychiatric nursing, drug therapy, and health education for both group, and additional tuina therapy for treatment group, for 2 weeks to 83 depression patients diagnosed by ICD-10 and corresponding to HAMD≥18. As a result, treatment group was reported to have significantly lower levels of HAMD and heart rate than control group, so they reported that additional tuina therapy has a significant effect to reduce depression and anxiety.
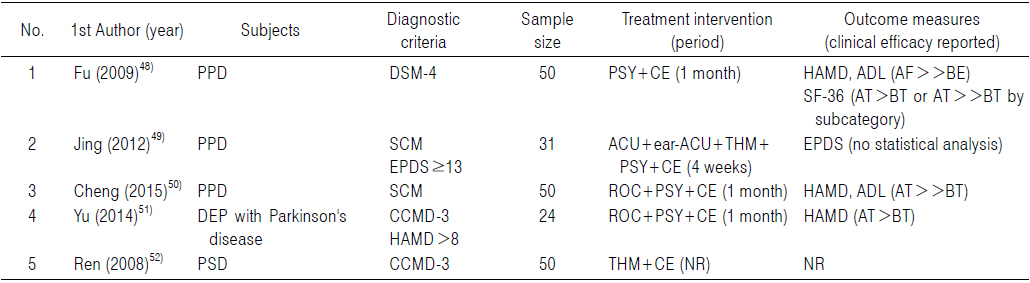
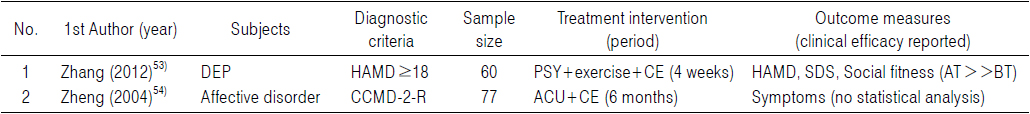
In case of 5 RCTs of depression comorbid with other conditions, studies about post stroke depression were 3 pieces, postpartum depression as 1 piece, and depression with peritoneal dialysis for chronic kidney disease uremia stage as 1 pieced followed. Zhuang (莊 子齊, 2004) performed acupuncture and tuina therapy once per 2 days for treatment group, and drug therapy for control group, for 1 month, to 62 post stroke depression patients diagnosed by CCMD and corresponding to HAMD>8. As a result, treatment group was reported to have significantly lower levels of HAMD and 1 year relapse rate than control group. Xiao (蕭蕙, 2008) performed rehabilitation care for both group, additional routine counseling for control group, and additional psychological care based on TCM and tuina therapy everyday for treatment group, for 1 month, to 150 post stroke depression patients diagnosed by CCMD and DSM, and corresponding to 35>HAMD>8. As a result, treatment group was reported to have significantly lower levels of HAMD, Activity of Daily Living Scale (ADL) and Short Form Health Survey (SF-36) than control group. Meng (孟慶芳, 2013) performed routine rehabilitation care and drug therapy for both group, and additional hyperbaric oxygen and tuina therapy everyday for treatment group, for 28 days, to 100 post stroke depression patients corresponding to HAMD≥17, NIHSS≥12. As a result, treatment group was reported to have significantly lower levels of HAMD, NIHSS, and Modified Barthel Index (MBI) than control group, so they reported that additional hyperbaric oxygen and tuina therapy have a significant effect not only to reduce depression but also to recover neurological disturbance. Qiu (邱豔麗, 2015) performed routine care for both group, and additional psychiatric nursing and tuina therapy once a day on hospitalization period and then 1 time per week, for 42 days, to 60 postpartum depression patients corresponding to EPDS≥10. As a result, treatment group was reported to have significantly lower levels of EPDS and PSQI and significantly higher levels of Quality of Life (QOL) and nursing satisfaction score than control group. Zhu (朱煒, 2014) performed routine care for chronic kidney disease for both group, and additional steam therapy on foot, eyepatch, and tuina therapy everyday for treatment group, for 40 days, to 107 depression patients with peritoneal dialysis for chronic kidney disease uremia stage corresponding to SDS>50, and classified as kidney deficiency and liver depression (腎虛肝鬱) and dual deficiency of the heart and spleen (心脾兩虛). As a result, there was no significant difference between two group until 20th day after treatment in PSQI and SDS, but at 40th day after treatment, treatment group was reported to have significantly lower levels of PSQI and SDS than control group (Tables 2∼4).
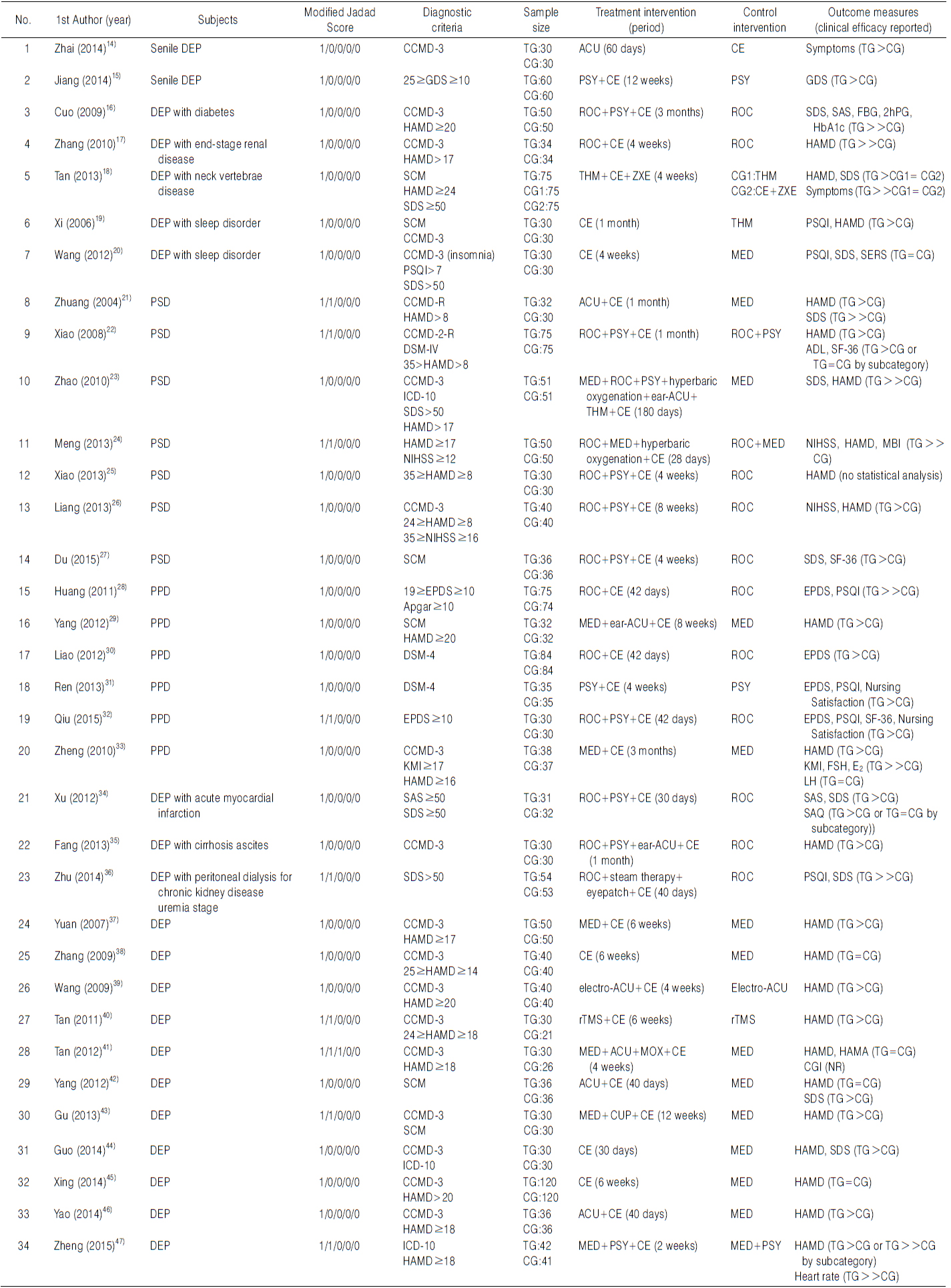
RCTs of Depression
[Table 3.] Prospective Studies of Depression Comorbid with Other Conditions
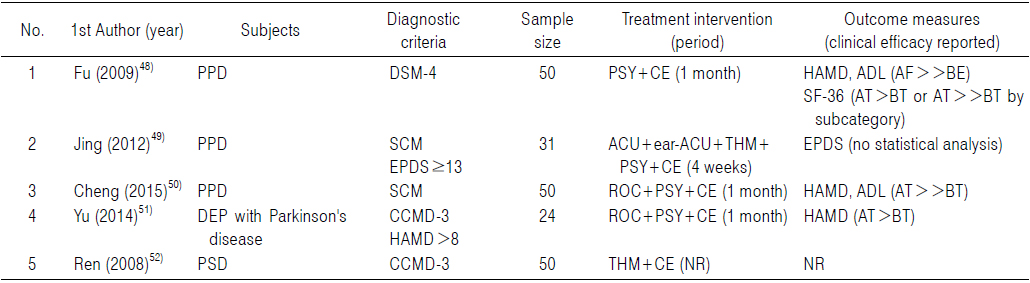
Prospective Studies of Depression Comorbid with Other Conditions
[Table 4.] Prospective Studies of Depression Comorbid with Other Conditions
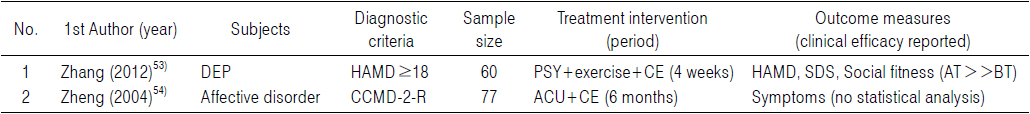
Prospective Studies of Depression Comorbid with Other Conditions
7. Example of performing tuina in a clinical field
For instance, one study, conducted by Tan (譚濤, 2012) and gained 3 points in modified Jadad scale, suggested the use of conduction exercise therapy as follows.
“For tuina therapy, a patient lies down in supine position and a doctor sits at the beside of the patient. At first, the doctor draw a straight line from Yin Tang (印堂, EX-HN3) to Bai Hui (百會, GV20) using qi-concentrated single-finger pushing manipulation (一指禅推法) for one minute. Then he rubs Yin Tang, Bai Hui, Tou Wei (頭維, ST8) and Feng Chi (風池, GB20) for one minute to get obtaining qi (得氣). And then he rubs from Cuan Zhu (攢竹, BL2) along the eyebrows and forehead to both temples, and applies acupressure Tai Yang (太陽, EX-HN5) and Yu Yao (魚腰, EX-HN4), using his both thenar eminence (大魚際) about nine times. After that, the doctor changes the position to the left of the patient, and rubs the patient’s abdomen clockwise for five minutes, placing his right palm on the patient’s Shen Que (神闕, CV8). Then again, rubbing in a counterclockwise for three minutes, he press gently the patient’s Quan Yuan (關元, CV4) until the patient feel warm on the abdomen and his both legs. Finally, the doctor acupress the patient’s San Yin Jiao (三陰交, SP6) and Jian Jing (肩井, GB21) for one minute, and press the patient's foot strongly with his thumb at Tai Chong (太衝, LR3) and his middle finger at Yong Quan (涌泉, KI1) about 9 times. After the therapy, the patient usually feels a warm feeling in the abdomen, and perceives a feeling of drowsiness.”
In this review, to investigate the researches about using tuina therapy for depression and to understand the efficacy, we searched clinical studies related with tuina therapy on depression at CNKI, Chinese database, selected and analyzed them. According to our criteria, by 1st screening with title and abstract and by full text screening, lastly 41 studies remained and examined tuina therapy for depression. As study types, they classified into RCTs and prospective studies, and we analyzed their contents and structure.
In contents of study, according to the content of diseases type, they were divided into 2 categories, studies of depression alone and studies of depression comorbid with other conditions, and in case of the latter type, post stroke depression and postpartum depression accounted a high percentage of subject. As a diagnostic criteria, most of studies used CCMD or DSM to diagnose depressive disorder, and as a screening tool, HAMD was the most commonly used. HAMD was also the most commonly used as a assessment tool to assess depression symptom, whereas EPDS and PSQI were used according to other conditions comorbid with depression to assess other symptoms.
To investigate the effect of tuina therapy more in detail, we classified tuina into two ways, conduction exercise and Zheng Xing exercise. All of 39 studies describing the method of tuina therapy used conduction exercise. Zheng Xing exercise was used in only 1 study of depression patients with neck vertebrae disease, but considering its subject, the method of tuina therapy on depression is mostly conduction exercise in fact. In case of the treatment period, frequency, and total time required to perform tuina therapy at one time, ‘more than 4 weeks, under 8 weeks’, ‘once per day’, and ‘more than 30minutes, under 1 hour’ were the most commonly used, respectively.
In structure of study, many of included RCTs performed common intervention for both group and additional intervention for treatment group. Among them, as a additional intervention, ‘tuina therapy combination with other interventions like acupuncture, traditional herbal medicine, and psychological intervention’ was the most commonly used. In case of prospective studies, ‘tuina therapy combination with other interventions’ was used totally as a intervention.
In result of study, in order to evaluate the quality of RCTs, modified Jadad scale was performed for 34 RCTs included in this review. And by assessing RCTs scored more than 2 points of modified Jadad scale, 4 RCTs of depression alone, and 5 RCTs of depression comorbid with other conditions were remained. In case of 4 RCTs of depression alone, HAMD was used for evaluating therapeutic effect of the intervention, and CCMD or ICD were used for diagnosing depressive disorder in all studies. And then the combination cares between ‘tuina therapy’ and ‘conventional treatment’ or ‘TCM therapy including tuina’ and ‘conventional treatment’, like rTMS, drug therapy, routine psychiatric nursing, and health education, were reported to have a significantly better effect for depression to reduce depressive symptoms and side effects. Among them, Tan (譚燚飛, 2001) reported that additional tuina therapy on rTMS 3 times per week seems to significantly increase the antidepressant effect of rTMS, and additional tuina therapy was particularly effective for the initial 1 month, which can be said to have meaning in clinical use.
In case of 5 RCTs of depression comorbid with other conditions, Zhuang (莊子齊, 2004) reported that additional acupuncture and tuina therapy on routine drug therapy seems to significantly reduce HAMD score and 1 year relapse rate than routine drug therapy alone. And in other studies also, additional tuina therapy on routine care such as counseling and rehabilitation reported to significantly reduce depressive symptom than routine care alone, when it applied to post stroke depression, postpartum depression, and depression with chronic kidney disease. Among them, Meng (孟慶芳, 2013) reported that additional hyperbaric oxygen and tuina therapy on routine rehabilitation care and drug therapy seems to have significant effect on neurological disturbance than routine care alone, when it applied to post stroke depression.
Depression, by its nature, has aspects that patients are reluctant to receive drug therapy, so nonpharmacological treatments are often used as complementary, and they are also known to have synergtic effect when they used with medication. Therefore its importance in the clinical field could be considered high. And in this respect, the clinical effects of manipulative therapies through physical contact like ‘therapeutic touch’12), ‘massage therapy’13) on depression have been reported.
In particular conduction exercise therapy used in all studies included in this review, can be used as the form of meridian massage or acupressure in clinical practice. These treatments, unlike typical massage therapy, have an advantage to provide patient-centered treatment based on TCM theory such as meridian and acupoint. As described above, tuina therapy has been recognized to be effective on depression in TCM, and it can be applied without difficulty in the clinical field. Therefore if the evidences supplementing the deficient quality of these studies are accumulated through high-quality studies, it can be considered as nonpharmacologic therapy for depression in Korean medicine, too.
The limitations of this study are as follows. Limitation of searching method limited to CNKI, limitation of composing detailed search strategy in Chinese, limitation of Chinese clinical trials laking ethics system like Institutional Review Board (IRB), limitation of high quality researches scored more than 4 points of modified Jadad scale, and limitation of selecting articles including depression patients by screening tool not diagnostic criteria.
However this study has meaning in terms of dealing with the effectiveness of tuina therapy on depression domestically for the first time. And it has a point that we investigated the study trend, and identified the effectiveness of tuina therapy on depression by assessing quality of RCTs. So it can be expected to be used in the progress of developing clinical guidelines related with depression as a data for determine the effectiveness of tuina therapy and as a reference for design of clinical research.
We investigated the study trend and identified the effectiveness of tuina on depression by searching relevant articles through the Chinese database CNKI. According to our inclusion criteria, 41 studies remained and examined tuina therapy for depression lastly, and the following conclusions were obtained.
1. RCTs occupied a high percentage (82.93%) among a total of 41 articles included in this review.
2. In case of 23 RCTs of depression comorbid with other conditions, post stroke depression was the most frequent subject (30.43%), and postpartum depression (21.74%) followed. And in 5 prospective studies, postpartum depression was the most frequent subject (60.00%).
3. Among the studies describing depressive disorder screening tool (57.14%), HAMD was the most commonly used (62.50%). Among the studies describing the assessment tool for depression symptom (95.12%), HAMD was the most commonly used (69.23%).
4. Among the studies describing the treatment period (97.56%), ‘more than 4 weeks, under 8 weeks’ was the most commonly used (60.00%). Among the studies describing the frequency of tuina therapy (85.37%), performing ‘once per day’ was the most commonly used (71.43%). Among the studies describing the total time required to perform tuina therapy (46.34%), ‘more than 30 minutes, under 1 hour’ was the most commonly used (78.95%).
5. Among the studies describing the method of massage therapy (95.12%), conduction exercise was used in all studies (100.00%), and Zheng Xing exercise was used in only 1 study (2.56%).
6. By assessing RCTs scored more than 2 points of modified Jadad scale, tuina therapy was reported to have a significantly better effect for depression to reduce depressive symptoms than conventional treatment. Moreover it was reported to increase the antidepressant effect when tuina therapy combined with conventional treatment additionally.