The purpose of this study is to report the clinical effect of Korean medicine (KM) treatment for Henoch-Schonlein purpura (HSP).
Five HSP patients who demonstrated a Yin deficiency and who had a history of a previous upper respiratory tract infection were included in this study. Four patients had arthritis and three had severe stomachache. One of them appeared to have proteinuria and hematuria before starting KM treatment.
All patients were improved with only herbal medicine, Jarotang (JRT). Purpura in the lower extremities and abdominal pain, which were not treated by using a corticosteroid, disappeared and had not recurred after 6 months.
These cases indicate that JRT may be effective in treating HSP in patients who demonstrate Yin deficiency, even though the number of cases was limited to five.
Henoch-Schonlein purpura (HSP), which is also called allergic purpura, anaphylactic purpura, is a kind of vasculitis and includes non-thrombocytopenic purpura, abdominal pain (AP), arthritis, and renal involvement [1, 2]. Its etiology is not clear, but the immune complex within the walls of small vessel is assumed to be related to HSP [3]. A virus or bacterial infection, drugs, itches, and food may be associated with HSP, considering a preceding upper respiratory infection [1-3]. HSP is common in children, especially children 4 to 6 years old, with a rate of 70.3 per 100,000 in children. The annual incidence of HSP is reported to be 13 to 20.4 per 10,000 population [2, 4].
HSP is characterized by purpura, arthritis, AP and glomerulonephritis [5, 6]. Conservative and steroid treatment is generally considered [5, 6]. However, steroids have been reported to have side effects [7, 8] and cannot improve or prevent purpura and nephritis [9, 10].
A few reviews [11, 12] and some case reports on HSP in view of Korean medicine can be found in the literature [8, 13-15]. For that reason, our purpose is to report five cases with Yin deficiency that were improved by using jarotang (JRT), a herbal medicine.
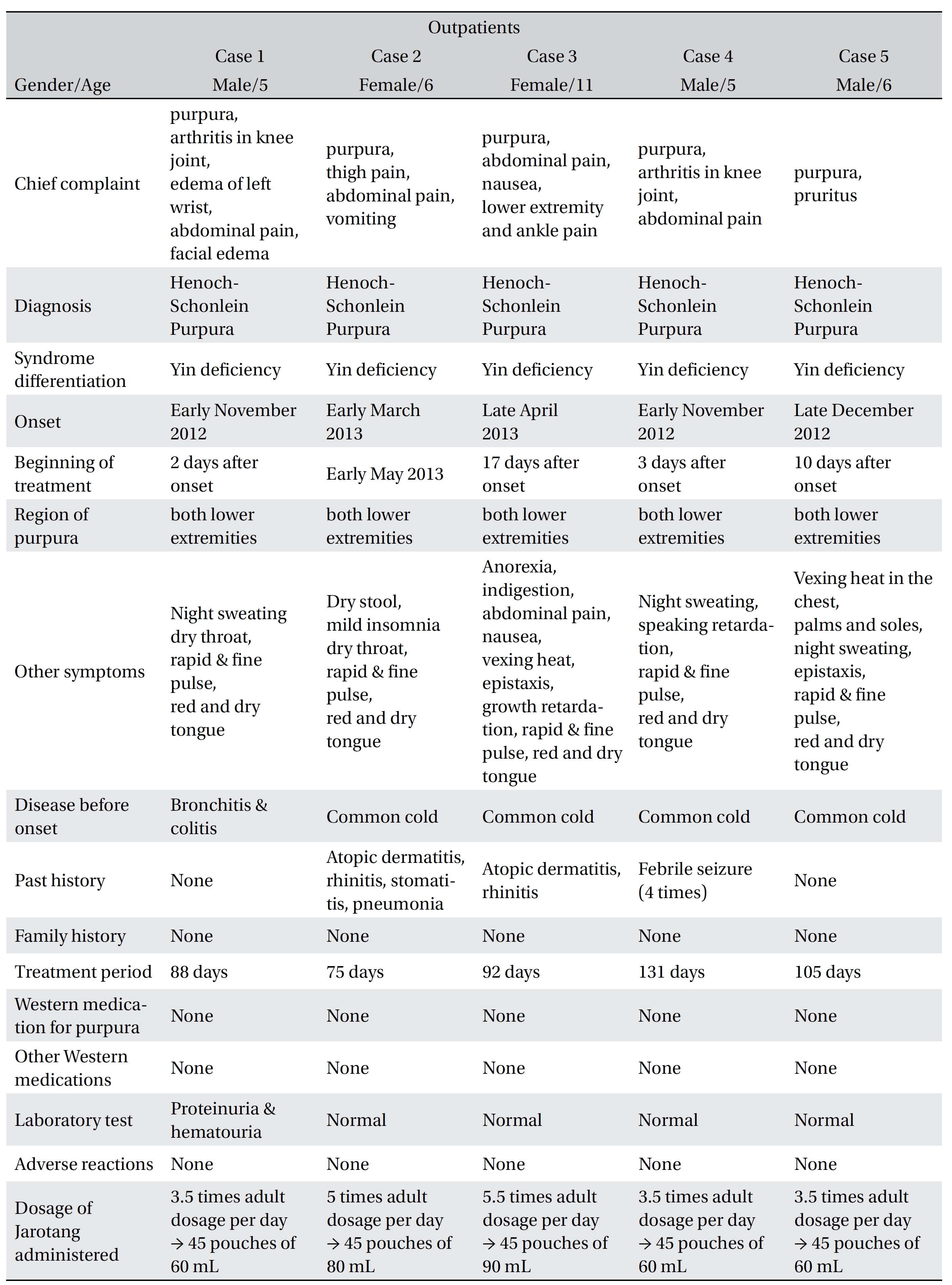
2.1. Characteristics of the patients and their medical history (Table
[Table. 1] Characteristics of the patients
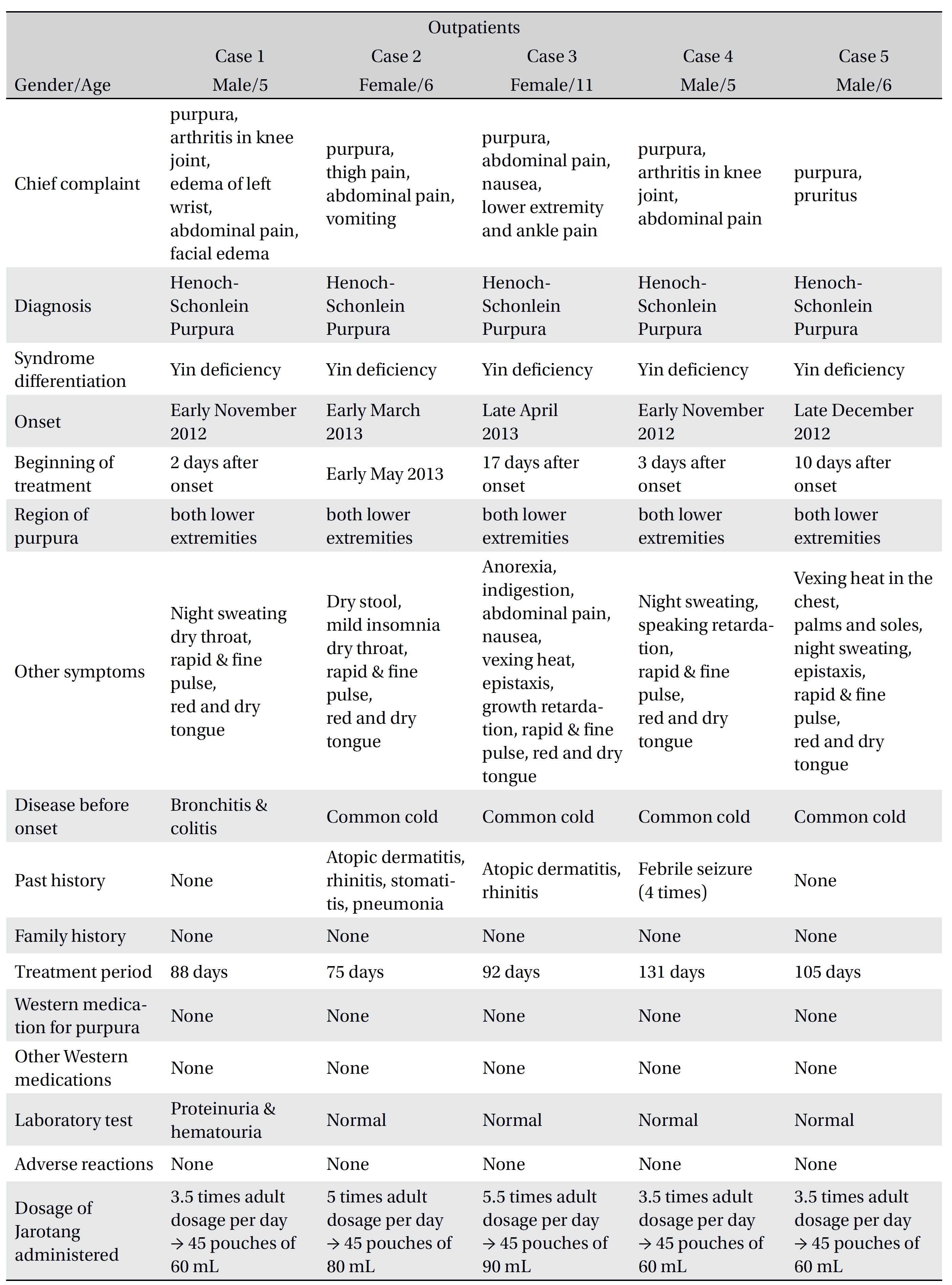
Characteristics of the patients
Case 1 was treated for bronchitis and gastroenteritis. After about a week, purpura of both lower extremities, arthritis in the knee joint, edema of the left wrist, AP and facial edema occurred.
Case 2 was being treated for a cold when purpura of the lower extremities and thigh pain with fatigue occurred. She was diagnosed with erythema. A cure was started, but no improvement was noted. She was also diagnosed as having HSP at another hospital and came to our clinic after a complete blood count (CBC) and urine analysis.
For case 3, purpura of the lower extremities occurred during treatment for a cold, and the patient was diagnosed as having HSP. The CBC was normal. For 3 days after admission, no improvement was noted, and a day after having been discharged, she was admitted to another university hospital because of sudden AP and nausea. On the second admission, purpura had disappeared, and other symptoms had also improved. However, purpura recurred after discharge from the second hospital, and she began to be treated at our clinic again.
Case 4 presented with purpura of the lower extremities after having had a cold. Severe arthritis in knee joint appeared after having taken corticosteroids for 3 days, and he visited our clinic.
Case 5 took antibiotics and a fever reducer for a cold, and after 10 days, purpura and pruritus occurred in the lower extremities. He was diagnosed as having HSP and began treatment at our clinic 10 days after the onset of symptoms.
All patients were demonstrated as having Yin deficiency and were diagnosed as having HSP at other hospitals. Case 2 and 3 had a history of allergic rhinitis, and case 4 had a history of febrile seizure. No patient had no family history of HSP or had received other treatments while undergoing Korean medicine treatment. Case 1 presented with slight proteinuria and hematuria.
JRT, 3.5 to 5.5 times the adult dosage per day, was decocted into 45 pouches of 60 to 90 mL by case. One JRT pouch was administered three times a day 30 minutes after each meal (Table 1). The dosage was adjusted in proportion to age [16]. No treatments other than herbal medicine were administered.
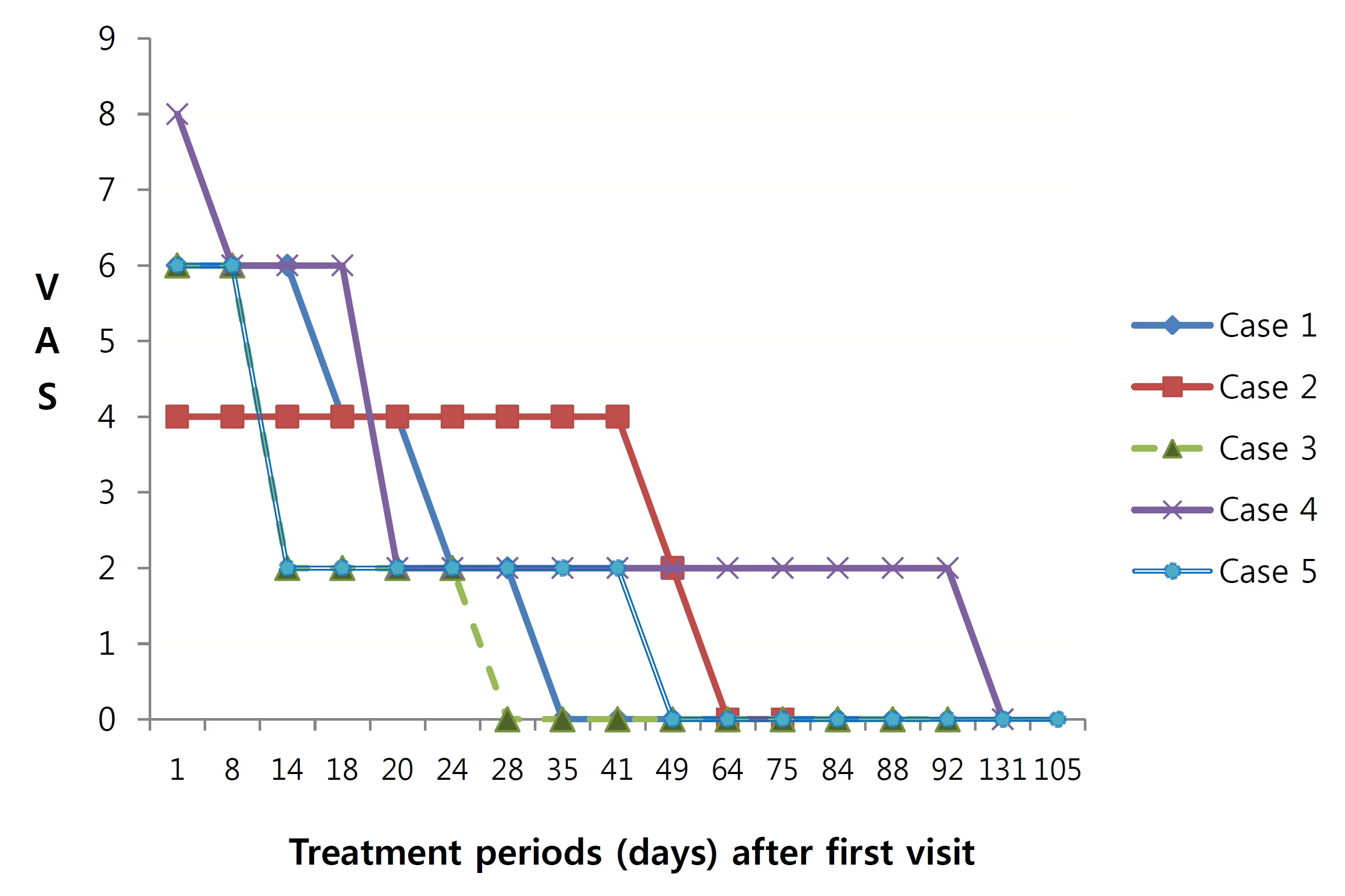
2.3. Progress of symptoms (Fig
Case 1 had purpura in both lower extremities and arthritis in the knee joint (visual analogue scale (VAS) 5) at the first visit. After 2 days, hand edema appeared, and after 5 days, he was admitted for a day because of sudden AP, facial purpura and edema. AP disappeared, but purpura in both lower extremities and the face still remained after 18 days. All symptoms disappeared after 35 days and had not recurred at the last visit.
Case 2 had purpura in both lower extremities and thigh pain (VAS 4). AP (VAS 3) and vomiting appeared 4 days after the first visit. The thigh pain and vomiting improved after taking JRT and disappeared after 14 days. Purpura also was improved after 49 days, and at 64 days after the first visit, none of the symptoms had recurred.
Case 3 had purpura in both lower extremities, AP and ankle pain (VAS 4). AP was relieved after 6 days and disappeared after 14 days. Purpura got worse temporarily, but disappeared after 28 days. AP recurred for 10 days, but again disappeared as well. Since the last treatment, none of the symptoms have recurred.
Case 4 had purpura in both lower extremities, arthritis in the knee joint and a gait disturbance. He was treated with corticosteroids and fasting for a day. Every symptom got better except AP. While taking herbal medicine, AP was reduced by half, and other symptoms began to improve in four days. Purpura almost disappeared after 20 days. AP re-appeared slightly with a cough and rhinorrhea for a cold, but disappeared. All the symptoms of HSP had disappeared at 131 days after the first visit.
Case 5 presented with purpura and mild pruritus at both lower extremities. Although HSP symptoms deteriorated briefly because of a cold, all symptoms improved after administration of herbal medicine. Purpura completely disappeared after 49 days, and did not recur after 84 days. At 105 days after the first visit, no symptoms had recurred.
All patients were administered herbal medicine for 75 − 131 days. No adverse reactions, such as indigestion, eruption, and so on, were observed.
HSP cannot be diagnosed by using an examination; reference must be made to clinical presentations and past history [3, 4]. Every subject in our study was a child between the ages of 5 an 11 years old and had purpura of the lower extremities, AP and arthritis. All of them began to be treated at our clinic after having been diagnosed as having HSP. HSP often follows a preceding upper respiratory tract infection, and all of the subjects in this study had a history of a preceding upper respiratory tract infection. Case 1 had bronchitis and enteritis.
The symptom differentiation of HSP can be classified as Blood heat and Blood stasis (血熱血瘀), Heat invading the collaterals (邪热傷), Yin deficiency and Blood stasis ( 陰虚血瘀), Qi deficiency with Blood stasis (氣虚血瘀), and Spleen-kidney Yang deficiency (脾腎兩虛). It is caused by Blood heat (血熱), Yin deficiency (陰虚), and Qi deficiency (氣虚) [11, 12]. All patients were demonstrated as having a Yin deficiency. Because children are full of Yang but lack of Yin (陽常有餘陰常不足), they easily go to a Yin deficiency. Yin deficiency makes effulgent fire (虛火), and purpura appears as a result of leaking blood with fire [11, 12]. All patients had signs of Yin deficiency, like night sweating, dry throat, red and dry tongue, and rapid and fine pulse.
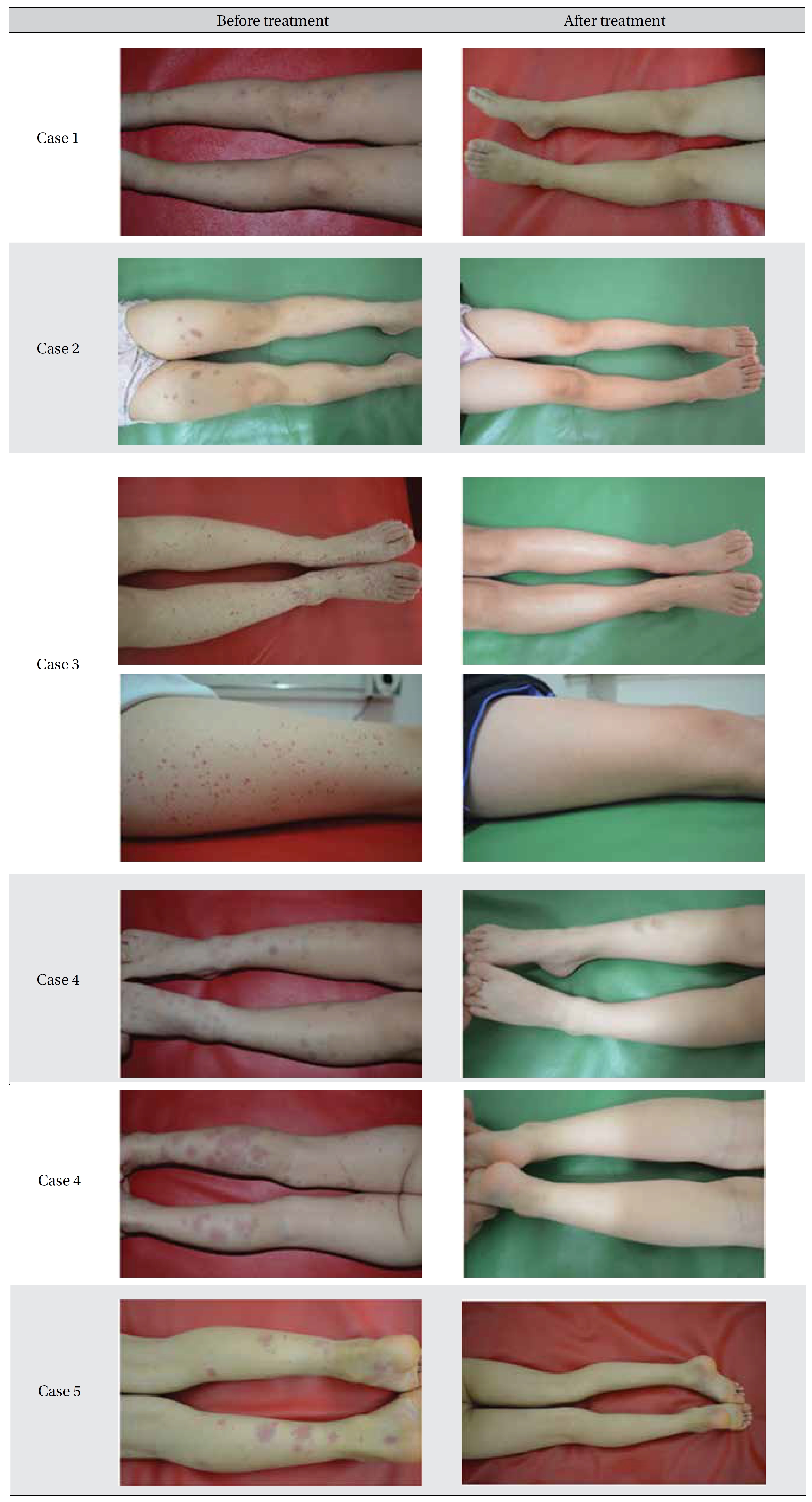
[Table. 2] Images before and after treatment
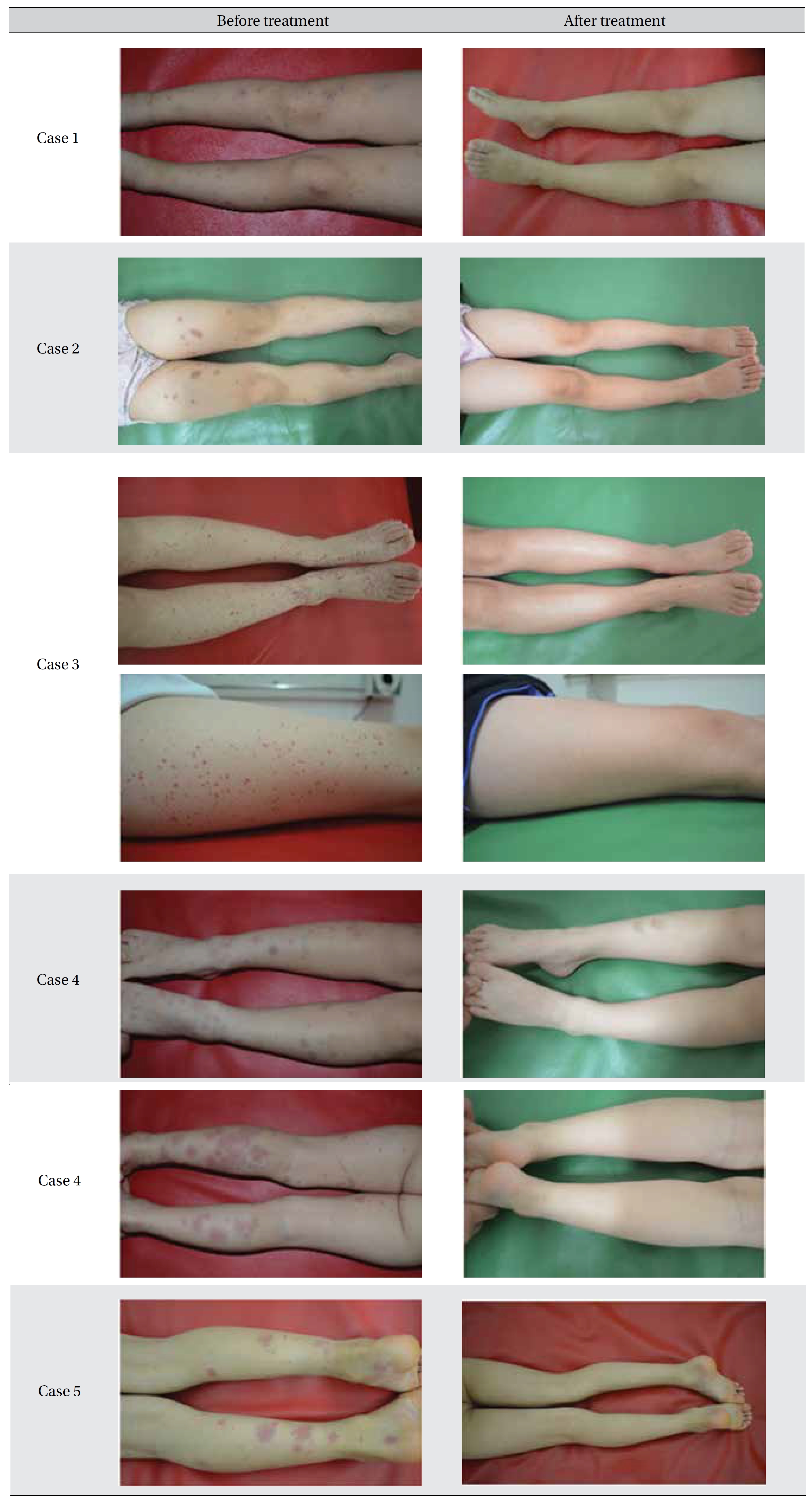
Images before and after treatment
JRT is a herbal medicine that adds Yukmijihwangtang (YMJHT) to Scrophulariae Radix to enrich Yin, down bear fire, clear heat and cool blood and to other medicinal herbs to dispense wind-heat. YMJHT is a typical prescription for Yin deficiency and is composed of Rehmanniae Radix Preparat, Corni Fructus, Dioscoreae Rhizoma, Poria (Hoelen), Alismatis Rhizoma and Moutan Cortex. JRT is likely to be a typical prescription for HSP because it is a herbal medicine that adds Yin-tonifying YMJHT to a Qi-tonifying medicinal (QTM, 補氣藥) and a blood heat-clearing medicinal (BHCM, 淸血熱藥). JRT tonifies Yin to settle effulgent fire down, and QTM stops bleeding as Qi tonifies because Qi controls blood (氣者血之帥). BHCM cools blood heat to settle down indiscreet acting of blood heat (血熱妄動) and inflammation. Thus, JRT treats HSP by tonifying Yin and Qi and by cooling blood heat. JRT produced improvements in all the patients with HSP.
According to a report, vasculitis of HSP can be in spontaneous remission, but in 20% − 54% of pediatric patients, it involves the kidneys, leading to the end stage of renal failure and renal disorders in 5% − 15% of such patients [16]. In that study, prednisone therapy was used for a maximum 3.5 months. That therapy reportedly led clinical recovery, but it had to be used within 2 weeks or had to be used selectively due to failure in reducing renal symptoms and to the risk of renal involvement [17-18].
Administrations of Korean medicine were varied from 4 − 6 days [14], 2 weeks [15], 6.7 weeks [8], 2.4 − 3.5 months [13]. In Chinese medicine, reportedly, vasculitis of HSP was treated from 2 weeks to 3 months and a combination with Western medicine was more effective. Therefore, the duration of administration in our study (except Case 4) was not considered to be too long comparatively. Although spontaneous remission may have occurred in this study, these cases are thought to show the effect of herbal medicine because the symptoms had mostly disappeared at times ranging from 28 to 131 days.
The results of this study cannot be generalized to all HSP patients because this is case report. Case 1 had proteinuria, which could be speculated as being due to HSP nephritis (HSPN), but we could not follow up after termination. However, our five HSP cases had all clearly improved as a result of administering herbal medicine without corticosteroids. No adverse reaction were noted, not even after taking the herbal medicine for a period of 75 − 131 days, and no relapse of purpura had occurred at times of up to 6 months after the end of treatment. The AP of Case 3 was improved by taking herbal medicine for 2 weeks, which was not controlled with corticosteroids. Thus, JRT could be effective and safe, and further research would be valuable because this study just reports five cases.
Because HSP can recur after 5 years, the patients must be followed. We believe that this study will contribute to the development of new drugs for treating HSP. However, well-designed, further clinical studies are needed.