The written case that reflects the course of treatment for a person is central to the East Asian medical tradition. This paper examines the approaches and particularities of producing the actual written account of the clinical encounter, or a particular aspect of a case, that may be required by acupuncture practitioners and researchers. It will discuss the influences that can be brought to bear on the construction and production of these accounts. In addition, it will outline and highlight historical approaches to the case record documentation process as well as debate the value and purpose of these. This paper aims both to assist the production of helpful and authoritative case records for practitioners and researchers, and to highlight the usefulness of such case records. Moreover, it will discuss not only why the case needs to be written and for whom, but also which agencies support and control what is written. How can contemporary requirements and traditional views both be incorporated accurately, with context and with meaning? The essence of this paper is that practitioner/patient interactions need to be documented, and it will explore how this can best be supported.
Acupuncture and moxibustion are often explored and disseminated through the use of cases. Cases are one of the main ways practitioners communicate knowledge. Farquhar (1994) and Furth et al. (2007) described a process of thinking with cases that lies at the heart of East Asian Medicine (EAM). Furthermore, cases can help to give a practitioner, or an educational centre, a sense of identity. Cases clearly are important and if their value is to be retained they need to be documented.
The following is an exploration, through the literature, of the production of case records as applicable to acupuncture practitioners today. It is often heard how time consuming this process of writing up practice is, but the evidence would seem to demonstrate the immense potential value of case records.
Records of any clinical encounter can fulfil many functions. Records enable a practitioner to give due consideration, to reflect on the interaction that took place and to plan present and future actions. Records also are for the patient, or any other agency, to be able to read what occurred in the session and ideally how the decisions were taken by the practitioner. Furthermore, records can allow acupuncture practice to be studied from a historical, social or cultural perspective and provide insight for everyone concerned.
Blalack (2010) suggests that case records have been a part of Chinese history for 2,300 years. Furth et al. (2007) asserts that narrative-style case records began to be produced and came to people’s attention during and after the Ming dynasty (1368 - 1643). Prior to this there had been a long history of some types of consultation records; Chunyi Yi (216 - 150 BCE) had compiled many cases in writing that were in the nature of a dialogue between doctor and patient. Some of these case records have survived in the historical text Shi ji (史記)
The naming of the written result of a practitioner/patient consultation in English has developed through many stages. From a historical perspective written information on patients were simply named Cases and differed in their content. These cases were written mostly for the personal information of the practitioner and publication. The requirements today are much wider than that. Among the more common terms for cases today are:
The case report perhaps denotes a shorter excerpt from a case record to demonstrate a particular aspect of the treatment or patient illness progression (positively or negatively). The case history relates more to the biomedical verbal assessment of a person. Furth (2007) refered to the use of the expression case statement but this can sound rather brief. Although the term patient notes clearly places the patient in the process, the word note can appear to rather undermine the importance of these cases, as if they were just jotted down in passing. There might also be the notion that patient notes may even have been written by the patient themselves. Case study is more of a research method, whereby a single case is analysed or a number of cases are compared, to uncover possible similarities, differences and relationships (Fish and Coles, 1998; Nester, 2004). This article is mainly about the written record rather than the process of gleaning information but is concerned that this written record is a true reflection of the multiple processes that form consultations and treatments. The term consultation record might be appropriate, but in order to avoid excluding the need to write up treatment sessions and to denote that the process of writing might continue outside of the time spent with a patient, the term case record has been chosen here.
1. The purpose of case records
Primarily the case record needs to hold information that will improve patient care; it is essential to value the importance of the patient in the case record. The idea that the person should never be excluded from the case is primary and this is what gives any case record the vital authenticity emphasized by Petraglia (2009).
Detailed descriptions allow practitioners to read through their findings in order to develop precise treatment goals that address a person’s main concerns (Donnelly, 2005). Such accounts can assist decision making, which is always an important part of practice; as Scheid (2002) asserts, case records are what we turn to in order to make our clinical judgements.
Also, case records are the way professionals communicate. A clear case record is vital, not only for other practitioners involved with the patient’s care but also for new practitioners taking over caseloads etc. Additionally, a good case record will support letters and reports more accurately to reflect what has occurred in the consultation and treatment sessions.
Furthermore, case records can be an invaluable source for learning and teaching (Blalack, 2010). The study of case records can help to bridge the gap between theory and practice for students and practitioners alike. Cases help to place theory in the context in which it is being used and stimulate questions about how health is embodied.
The case record is also a legal document and as such there are legal obligations.
Finally, case records have always been a way to develop publications and undertake research. The idea of the case as relevant can be seen for example in interpretive case studies with case records forming the data of choice in much current research (Liu et al., 2012). This current thinking places the individual case in higher profile, and methods for evaluation, such as case study and case series, are becoming more commonly accepted (Nester, 2004; Prakash et al., 2012). Nester (2004) describes case study when referring to research using individual cases and the case series style of research whereby a number of cases are compared, often under different conditions e.g. single case study research.
Through all these ways, as a result of self-disciplined attention to good patient records, a cycle can be completed that supports the foundation for general dissemination of information on acupuncture practice.
2. The value of details and reflection in action on the page
The case record aims to detail what has taken place in the clinical encounter and to be a true reflection of this; thus the case should be both a descriptive account and a reflective account. Written case records seek to reveal the patients’ perspectives on their experiences of illness. Thus, language for case records ought to be appropriately sensitive to the patient’s concerns and written from their perspective, as well as being the reflections of the practitioner and involve in their construction reflection in action. Reflection in action here refers to the collection of information and encourages practitioners to see patterns and explore these possibilities, not only after the consultation, but also continually throughout the process of examination. It is important to make these findings explicit in the case record.
The language used in a case record needs to be readable but not lacking sufficient detail to be an accurate record. Indeed, as (Kleinman, 1988) explains ‘for the chronically ill, details are all’. Additionally, Cassidy (2002) pointed out EAM expects any information to often be in minute detail. Importantly, the detail in the case record must reveal what the practitioner has observed, what they smelt, what they heard, what they thought, as well as what the patient has actually said. The importance of writing down these clinical cues, derived from the sì (四) zhěn (診) methods of examination, is to continue to value, in EAM terms, this type of material as essential. This approach reflects what the sociologist of science Bruno Latour recommends for finding ways to describe complexity in words (Latour, 1999).
Finally, it is not really appropriate to use in case records language that contains humour or irony, nor that is in any way disparaging of the patient or other professionals.
3. The description of the process, including ideas and reservations
The legal aspects of what is documented must not be the only consideration as regards how the intervention is described.
The case record ideally reveals a window into the practitioner’s thinking; a sense of what were the lĭ (理), fă (法), and yì (意) [principles, strategies and reason or rectification, methods and the ability to grasp (Scheid, 2002)] behind the differentiations [e.g. biàn bìng (辨病); biàn zhèng (辨证); jīng (经) lùo (絡), etc] and prescriptions. Farquhar (1994) explained sometimes referred to as kan bing (看病). The initial impressions need to be documented and given value.
Furthermore, the case record might discuss the insights or intuitions experienced by the practitioner at any stage during the practitioner/patient interaction, always giving information on the clinical thought processes. The practitioner needs to feel free to write down ideas and anxieties in an open professional fashion.
4. Stories, narratives and dialogue
The manner in which ancient cases were written as dialogue is reflected in the present-day interest in narratives, and many similarities can be seen. In addition, Jiao (2006) maintained that information is gathered at the time that it is given and that any information given by the patient might be pertinent to understanding their concerns and may inform treatment.
When documenting narratives, it is not only key words that can be highlighted in the notes but also the actual words/sentences used by the patient. The aim is to obtain sufficient information to construct a storied case record. Construction here means an interpretation of the narrative of the illness experience: not a reductionist perspective on the particulars but an interpretation that is wide-ranging, building a complete and consistent meaning. This construction will involve truthfulness; sincerity; integrity; trustworthiness; dynamism and pattern recognition by the practitioner and the patient. In order to encourage narratives, practitioners need to build rapport, develop styles of communication and skills, in both asking questions and listening to responses. Appropriate space and sufficient time are needed to do justice to these approaches and to allow patients to tell stories, recollect with accuracy and express their emotions (Bury, 2001; Charmaz, 1999; Charon, 1992; Greenhalgh and Hurwitz, 1999; Hydén, 1997; Kleinman, 1988; Macnaughton and Evans, 2004; Mattingly, 1998).
Carson (2001) stated that it is important to remember that case records are themselves social constructions and that they will produce their own realities. With this in mind, a need to focus on the best possible way of keeping the patient and their needs at the centre is evident. Carson (2001) further suggested that narrative methods ‘remind us that behind every practice, there is a person, waiting to be heard’.
5. Ethics, metaphysics and informed consent
Ethics is considered to be at the heart of all interactions with patients. Tauber (2002) encouraged the ethical contribution in the case history at all stages, indeed he suggests that the debate on what constitutes good case histories cannot be entered into without due consideration of ethical issues. This paper presupposes that everyone starts from the same normative ethics. However, it also acknowledges that everyone is also constrained, as well as supported by, institutions, social structures, politics and nature.
In order to explore what ethics is, it is often considered to be interchangeable with morals and a call for moral behaviour to support ethical behaviour and vice versa would seem obvious (
Fortunately, there is much in EAM metaphysical philosophy that is related to methods of thinking to support ethical and moral behaviour. Once more, the need to acknowledge and document these thinking processes is worth consideration.
It is often considered that the ethical issue of informed consent relates only to the administration of a treatment. However, the whole interaction of the examination and case history taking and the documentation itself, requires that patients are informed of what is happening and what will be happening with the information they are divulging. Patients need to know who will be able to directly access the notes e.g. colleagues working together, and who will not. Confidentiality, Stone (2002) asserted that they are very important and includes respect for the value of professional relationships. Records must only ever be used for the purposes for which they were intended and no information should ever be given to any commercial organisation of any kind. Revealing case records in the UK can only be allowed with the patient’s consent, with a few exceptions. The exceptions include instances when in the practitioner’s considered opinion the person might be a danger to themselves or others. Troublingly, in legal cases in the UK, where once a practitioner’s letter or written report on a patient was accepted, today solicitors are increasingly asking for full photocopied notes, a practice that brings up issues of disclosure and confidentiality. A patient’s notes, particularly in this East Asian Medical tradition, can contain enormous detail. Much of the detail in a case record may be unrelated to the particular legal case. Furthermore, any patient may have been under treatment when the accident/incident occurred for which they are being sued or taking action against. In this situation, the treatment resulting from this accident/incident may only take up part of the treatment administered.
Documentation of informed consent may be important, but this can never replace the ongoing process of patient/ practitioner interaction, generating that continuous consent.
The case record may be recorded manually on either preprinted sheets or plain paper in legible writing. Most useful are probably pre-printed sheets for essential information, medications, outcome measures etc. as required, but also plain/ lined paper to encourage expression (Tables 1-3).
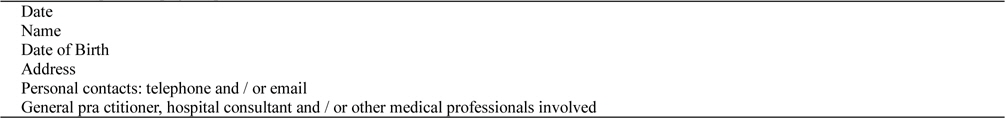
[Table 1.] Example front page of patient record sheets
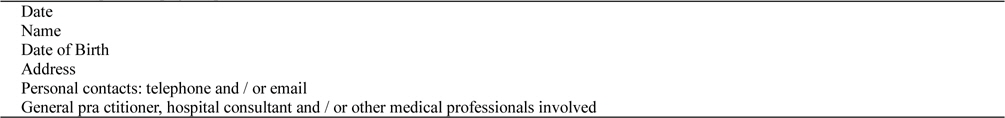
Example front page of patient record sheets
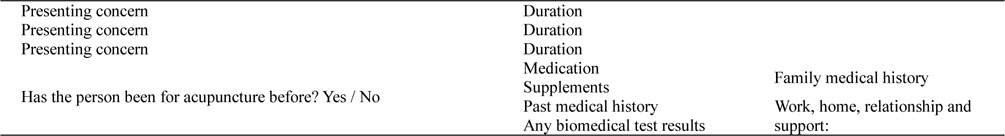
[Table 2.] Record of initial consultation
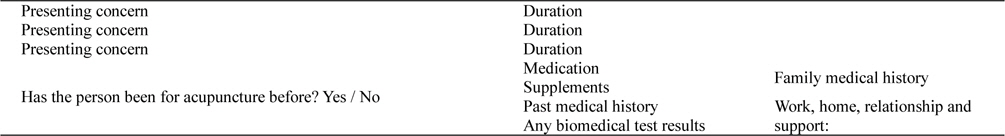
Record of initial consultation
[Table 3.] Format for minimum ongoing records

Format for minimum ongoing records
In addition to the extensive information needed to be able to discern what occurred during a patient/practitioner consultation, a good case record will also have the following:
6.1. Essential information
Initially comes the personal profile of the person and might include different information, however, Table 1 shows an example of a standard front page. Table 2 can be used to document the initial consultation and may contain the following information.
6.2. Personal information
Includes who this person is, what their personal circumstances are, and what their social context is. Some indication as to their aspirations in respect of their own health and wellbeing as well as their medical self is required here.
Dependingonthe severity of the main concern details might need to be taken of family medical history. However, brief attention given to family history in all patients is often helpful to the construction of a case record.
Moreover, the person’s lifestyle needs to be documented. Do they smoke, drink alcohol or coffee? What are their daily habits, food, work, rest and relaxation? Careful questioning, using introductory open questions such as ‘tell me something about .’, is required to overcome patients’ repeating oft told (and often ignored) stories, and to construct anew the patient’s own personal story.
6.3. Past medical history, test results and medications
Patients’ past medical history is so often related to their current complaint that details need to be taken. Past operations, illnesses, conditions etc., the details of which can be asked initially with open questions and then further explored, can be elicited and documented. If patients have had any tests e.g. x-rays/ scans/blood tests, ECG’s etc. carried out, then this too can be recorded, along with the results if possible.
It is always important that a complete and up-to-date record be kept of medication currently being taken, and this ought to include the dosages as well; a copy of this may be kept on a separate sheet in the case record. Medication would include recreational drug use (where possible to assert) as well as consumption of herbal remedies or supplements.
6.4. The case-taking information and differentiation process
The whole diagnostic process of sì (四) zhěn (診) should be documented. The signs and symptoms need to be organized to support the conclusions and the whole process needs to have transparency.
The differentiation may have a number of conclusions that uphold what Unschuld (2006) described as the balance between ‘A categorising and an individualising approach’. The written record should include detailed explanations of the treatment principles and strategies e.g. of the bĕn (本) and biāo (标) of the case and the reasons behind the priorities for treatment. Only in this way will the case record, once complete, show the rationale for proceeding.
The case record must document both initial consultations as well as any follow up appointments and/or treatments.
6.5. The intervention
Details of any needles inserted must be recorded at every session in the UK. A fuller description of the treatment given is boundlessly advantageous. Many of the details required might be appropriately similar to those set out by MacPherson et al. (2002) in the Standards for reporting interventions in controlled trials of acupuncture guidelines. These include: The specific points used (ideally these points will be written in both numerical form and named).Angle of insertion and depth of needling using the proportional measurement of cun.Type of needles and size of needles used.The total number of needles in the prescription.Point classifications, and/or why the points were chosen.Techniques used on the needles and the length of time the needles are left in.Any adjuncts used such as moxibustion, cupping or plum blossom needling etc.
Of interest to note may be any reactions observed or heard, as well as any sensations described by the patients, such as: “tingling, like water trickling down, like electricity shooting, spreading ache”; etc.
6.6. Legal requirements
Case records can be used as a legal document e.g. the case record may be required as evidence in a court of law. Consequently, the case record is not only a source of valuable professional information, but also potentially an important public document. As such, written case records need to be kept in permanent ink and Stone (2002) defied that the date should be written on every entry in the record. The author/authors of case records need to be made apparent. Ongoing records thus need to be kept with at least the minimum requirements (Table 3).
Records can be either kept as a hard copy in a file and stored in a filing system or kept in electronic/digital form. All storage of patient records raises the question of data protection but if kept electronically special procedures must be followed. Two points to highlight here are that in the UK you are legally required to retain patient records for a minimum of seven years and your patients’ case notes and records are your property that you must keep. Feng et al. (2006) suggested that there may be great advantages to electronic records, such as storage, sharing and data analysis, but this trend needs to be carefully monitored and researched if nothing is to be lost, as Macnaughton (2004) suggested that writing electronic notes during a consultation greatly reduces both the patient’s and the practitioner’s voice.
8. Outcome measures, referrals and advice
In effective health care, evaluating practice is a major social issue. One way of evaluating practice is by the use of outcome measures (OM). Baumberg et al. (1995) stated that an OM shows the results of healthcare processes. Evaluation of treatment outcomes can help to plan treatment and help to progress treatment efficiently.
Outcome measures cover both those measures that are carried out by clinicians in the treatment room, and those that would be carried out in hospitals and other assessment centres. It can be appropriate to use subjective measures such as Measure Yourself Medical Outcome Profile (MYMOP) as a validated outcome measure as well as other valid and reliable outcome scales. In addition, more defined objective measures such as blood pressure, blood tests, X-rays etc. Paterson and Britten (2003) may also be appropriate and helpful.
However, outcome measures in EAM need to take into consideration not only standard measures of pain and functionality etc. but also the energy levels or the feeling of health and wellbeing experienced by the patient. In addition, factors such as improved self-esteem, greater confidence, return to work, change in behaviour and mortality can all be valid measurements of treatment outcome. This demonstrates the range of measurements including values, beliefs, behaviours and actions that may be included as OM’s. Some of these relatively new dimensions of measurement equate more closely with the patient experience and this is another valid reason to use them to measure treatment success.
In research, there is the possibility to consider, as well as the choice of outcome measures, when these measures are performed. In order to demonstrate the effects of acupuncture, it is essential that long term follow-up of outcome measures is undertaken. MacPherson and Fitter (1998) suggested that six months is a suitable time to continue with outcome measures after treatment has stopped, however Paterson and Britten (2003) suggested this as a minimum time. Interestingly, the back pain research carried out by Prady et al. (2007) showed statistical improvement (in the acupuncture group over the control group) only after two years.
Finally, note any action or referrals suggested, and keep copies of any letters written or advice given to patients.
There are many benefits of a good case record, but essentially they can help to ensure good patient care. The case record is not only a way to detail facts; it can also make explicit to the reader how decisions are taken in clinical practice. To this end, useful case records give some context and meaning, illuminating the processes of diagnosis and treatment. Written case records help to place theory in the context in which it is being used. A case record aims to present a credible representation of reality, a sense of what took place. According to the use to which the particular case will be put, certain aspects of the information will be emphasised, whilst others will be less central.
Constructing case records effectively and accurately requires self-discipline on the part of practitioners and may not always be feasible. But case records constructed in this way will help to provide the possibility for understanding of what actually happens in EAM clinical encounters. At this time it is particularly important that good case records can be made available so that acupuncture and moxibustion practices can be made transparent and better understood by the general public, other health professionals, the legal profession and relevant regulatory bodies. However, principally it is to strive to ensure best patient care that good case records need to be written.