Of the cancer-related symptoms, cancer pain is a long-standing and unresolved clinical problem. It has been several decades since the World Health Organization (WHO) came up with the analgesic ladder for pain control, but cancer pain still remains one of the most distressing symptoms for cancer patients [1]. According to a meta-analysis on cancer pain, about half of all cancer patients suffer from cancer-related pain [2], and more than 90% of cancer patients have experienced cancer pain at some points during their treatment for cancer [3].
Acupuncture, a traditional Oriental medicine modality, is used in supportive care for cancer pain [4, 5]. Pharmacopuncture is a relatively new form of acupuncture treatment combining meridian-theory-based acupuncture and herbal therapy. While existing acupuncture treatment incorporates physical stimulation of associated meridians and acupoints, pharmacopuncture adds the medicinal effect of herbs injected to the regular effect of acupuncture. Similar to pharmacopuncture is Chinese aqua-acupuncture and European homeopathy. The concept of pharmacopuncture was first introduced to Korea in 1967, and many herbal injections have been researched and developed since then [
Autonomic nerve pharmacopuncture (ANP) is a subcutaneous injection therapy of mountain ginseng pharmacopuncture along the acupoints on the spine (Hua-Tuo- Jia-Ji-Xue) to enhance the immune system and to balance autonomic nerve function. It contains various flavonoid components from distilled mountain ginseng extract. To briefly explain the process of making mountain ginseng pharmacopuncture, 100 g of wild mountain ginseng is decocted in distilled water for 2 hours, and the decoction is distilled to produce 1,000 mL of pharmacopuncture fluid, which, in turn, is filtered with 0.45-μm and 0.2-μm filters and sterilized in vials [
This case involved a 41-year-old female patient with a weight of 46.5 kg and a height of 161 cm. The initial diagnosis was made in August, 2011. The pathological diagnosis showed a signet ring cell carcinoma, with chronic mild superficial gastritis. Biopsy revealed a moderately-differentiated tubular adenocarcinoma. The primary lesion was located in the middle third of the stomach (center at the body’s anterior wall). Initially 5 of 59 lymph nodes were positive, and metastases were present in the periportal area, Rt. periureter, ascending colon, and transverse colon. The initial stage of the cancer was IIB (pT2N2); the present stage is IV. A total gastrectomy was performed on September 1, 2011, and chemotherapy was administered from December 2011 to July 2012 (a total of 6 times). Common complaints were abdominal pain, diarrhea, nausea, and fatigue. A gastric ulcer had been noted around the year 2000. Adhesion and obstruction of the small bowel were also noted, and surgery was performed on September 8, 2011.
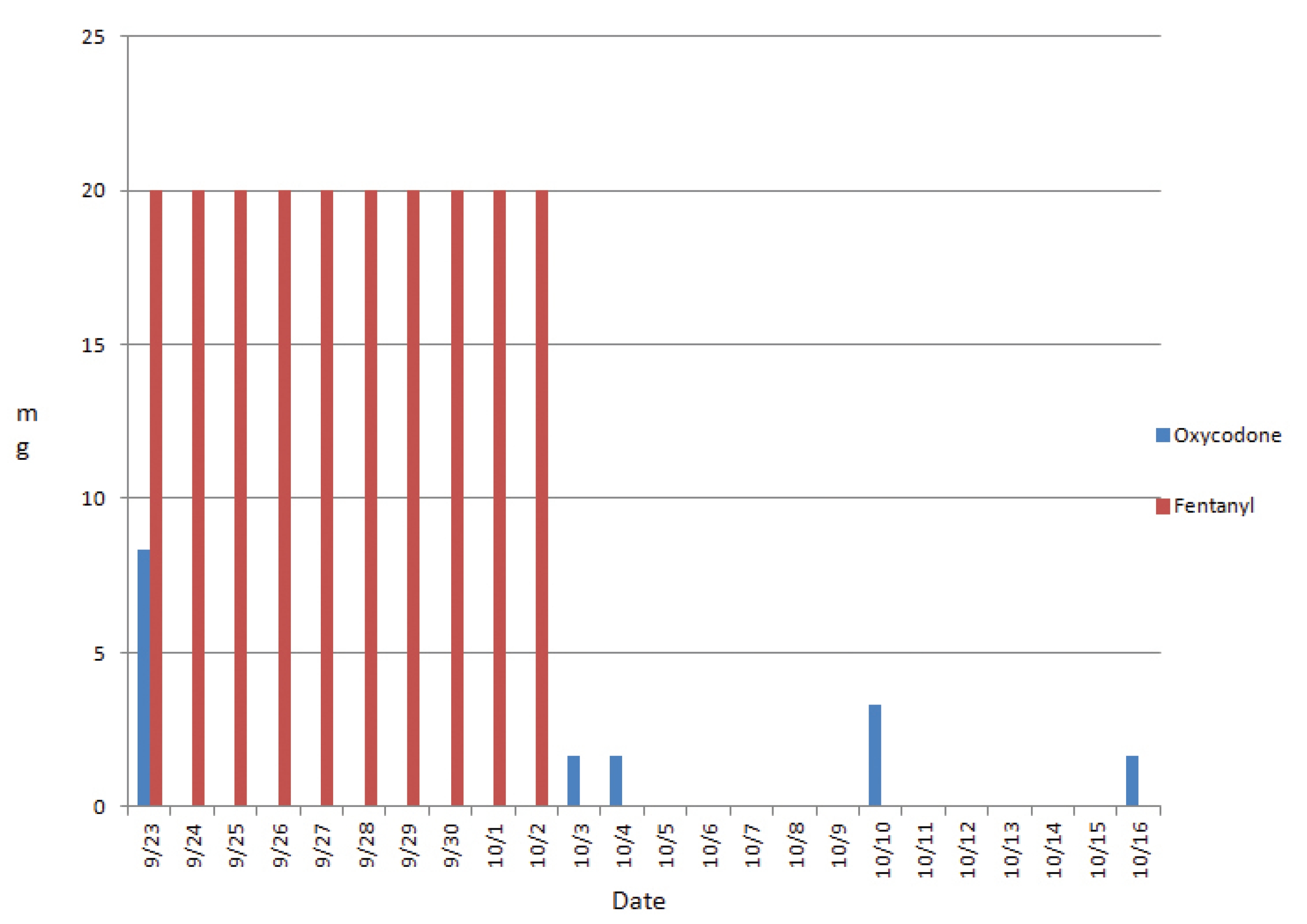
From September 2, 2013, to October 17, 2013, the patients received acupuncture and ANP treatments, as well as analgesiacs. Acupuncture was administered once a day for 15 minutes each time at acupoints LI11, TE5, LI4, SP10, SP9, ST36, SP6, and LR3. ANP was administered from September 23, 2013, to October 15, 2013, for a total of 20 times. Analgesics included oxycodone hydrochloride (5 mg) and fentanyl (25 mcg/hr).
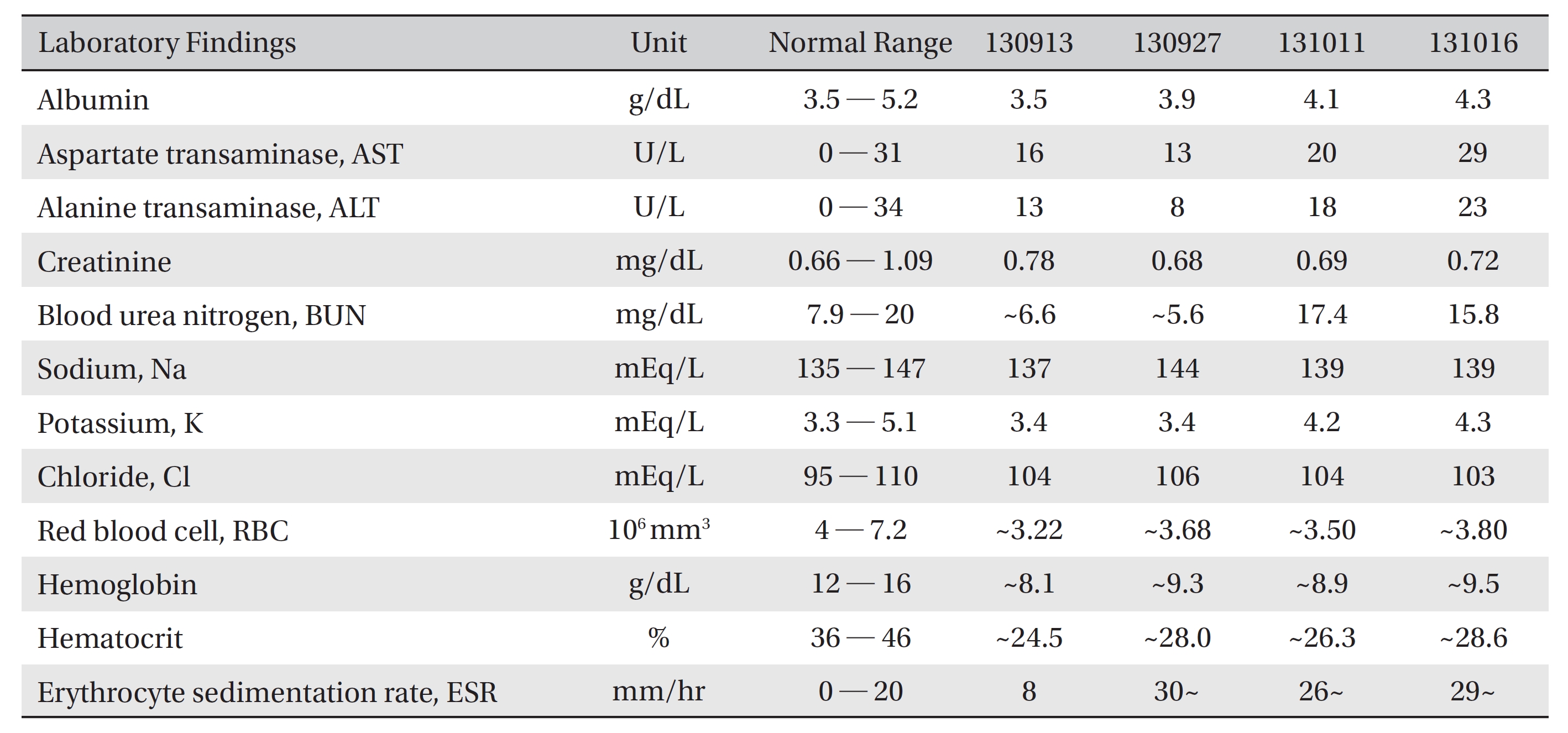
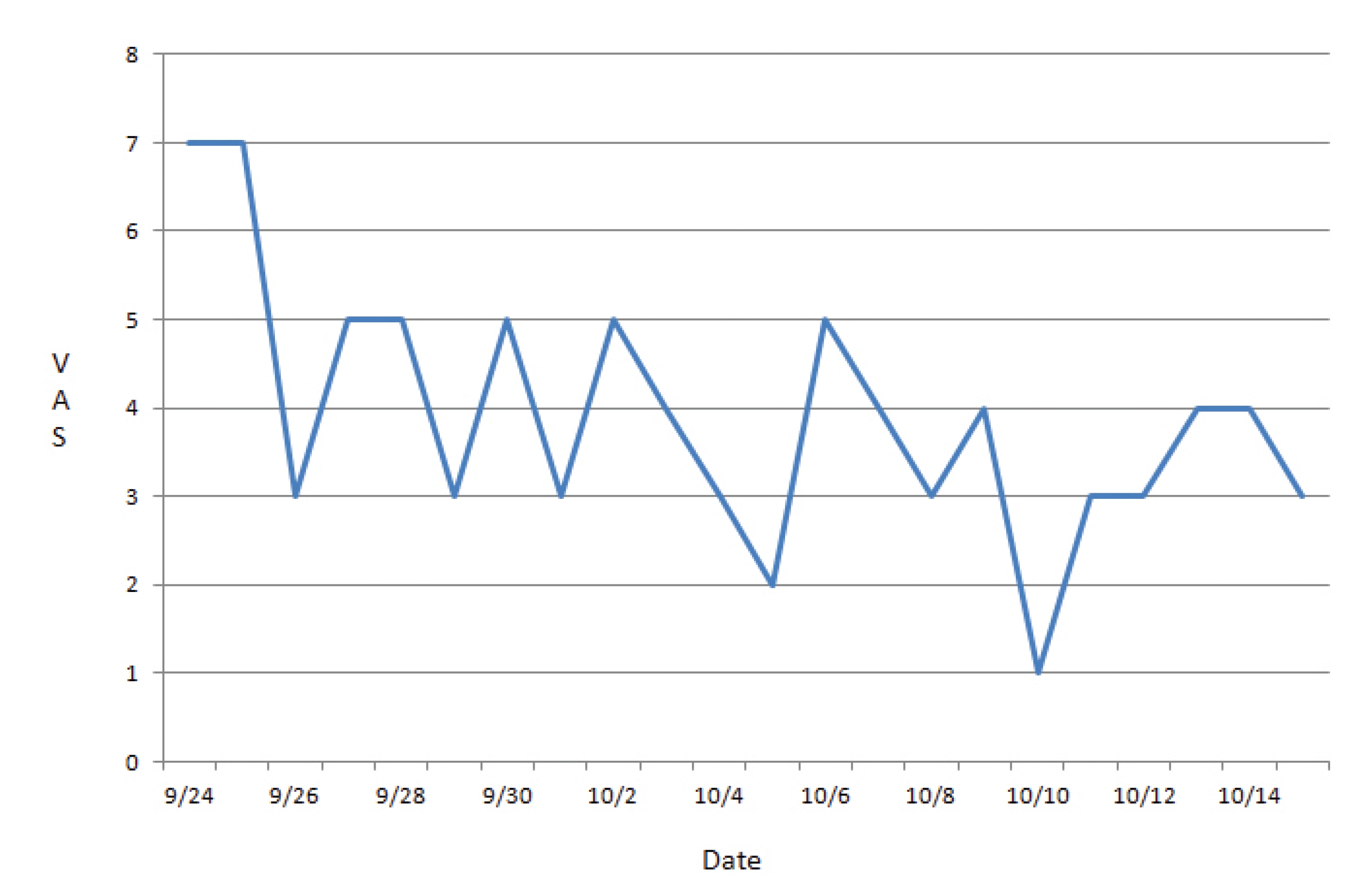
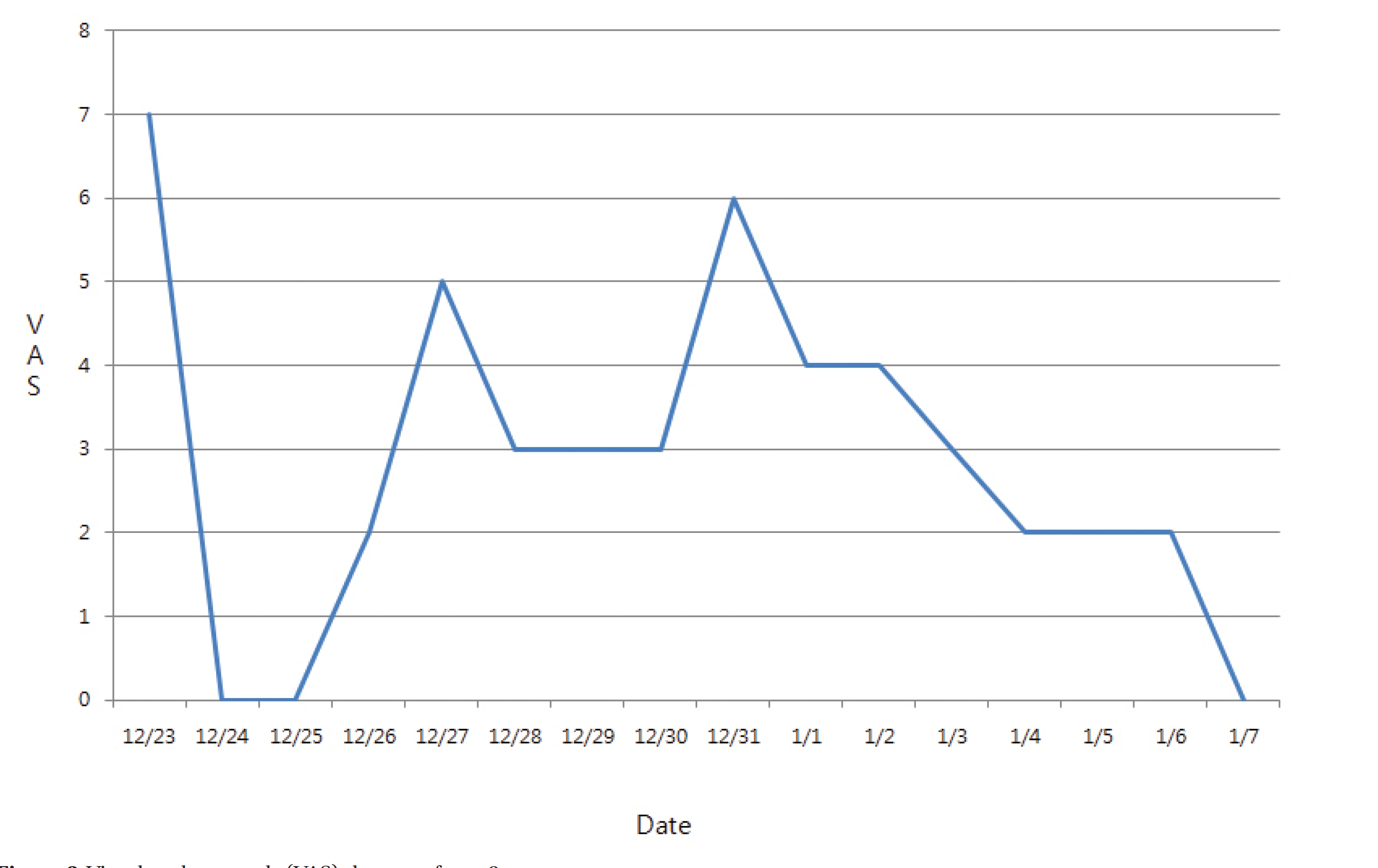
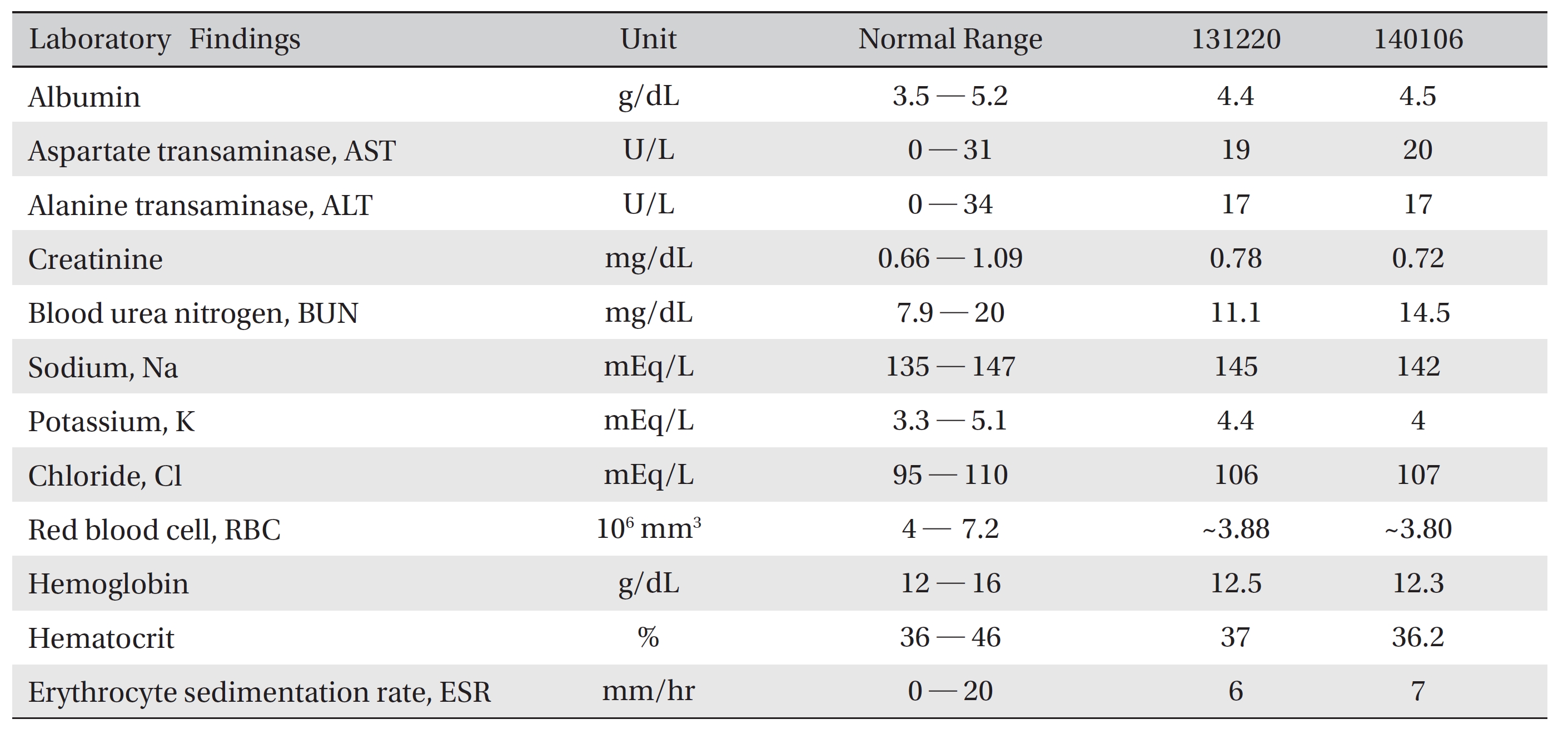
This patient was initially diagnosed with advanced gastric cancer, which later metastasized to the large intestines in April 2012. The patient refused chemotherapy and only received traditional Korean medicine treatment. Her main complaints were right abdominal tenderness with diarrhea, colicky pain in the ascending and the transverse colon, epigastric bloating after meals and heartburns at night. These different types of pain in multiple sites are common in patients with intraperitoneal metastases as infiltration, compression and distention in the intra-abdominal and the pelvic-cavity regions can stimulate nociceptors and lead to visceral pain. Paralytic ileus caused by opioid analgesics and disturbance of the peritoneal blood supply were also considered to be factors affecting her severe sporadic abdominal pain. At the time of admission, the patient was using opioid analgesics (oxycodone and fentanyl patch) for pain control. After admission, 10 days into receiving the ANP, the patient was able to stop using the fentanyl transdermal patch (25 mcg/hr) and to reduce the amount of oral oxycodone (5-mg tablets) to 1 ─ 2 tablets a day. The visual analogue scale (VAS) score declined from 7 to 3. With the decreased use of opioid analgesics, adverse effects, such as sedation and nausea, were also improved (Table 1), (Figs 1,2).
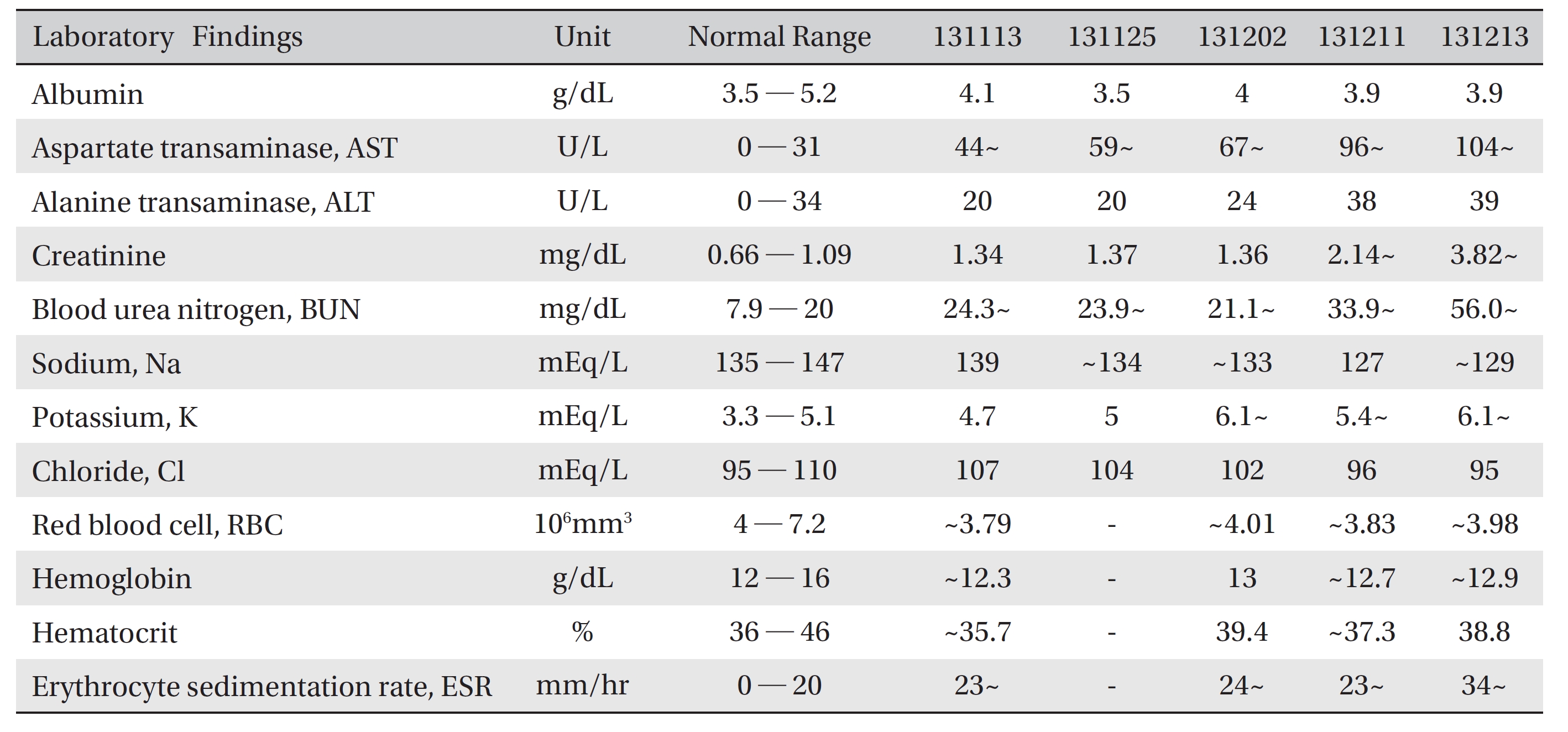
[Table. 1] Laboratory findings (case 1)
Laboratory findings (case 1)
This case involved a 51-year-old female patient, with a weight of 63 kg and a height of 160 cm. The initial diagnosis was made in January 2010; the pathological diagnosis showed a bronchioalveolar carcinoma, and biopsy revealed an adenocarcinoma. The primary lesion was located in the right upper lobe (RUL) of the lung. Initially no lymph nodes tested positive, but metastasis– was found in the Rt. pleura in February 2013. The initial stage of the cancer was IA (TNM: pT1bN0), and the present stage is IV. A RUL lobectomy and a wedge resection of the right middle lobe (RML) were performed on February 16, 2010, and chemotherapy was administered from February 21, 2013, to the present (p.o. Iressa). Common complaints were dizziness, nausea, vomiting, insomnia, fatigue, diarrhea, and dyspnea.
Medications included Iressa (Gefitinib) 250 mg 1-0-0 antineoplastics. Pulmonary tuberculosis (Rt. lung) was diagnosed in 2008.
The patients was admitted from December 9, 2013, to January 7, 2014, and ANP was administered from December 23, 2013, to January 2, 2014, for a total of 5 times. No analgesics were used.
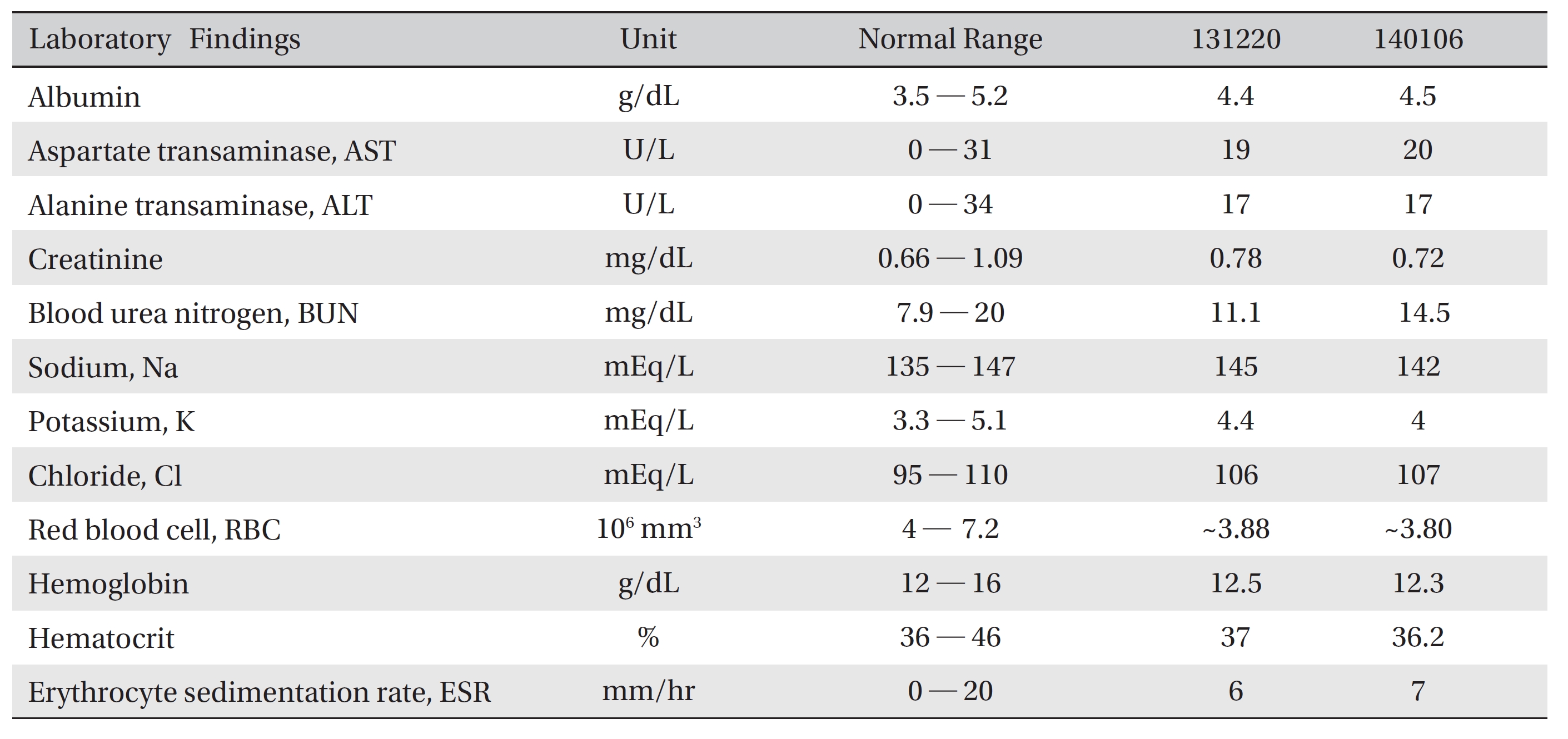
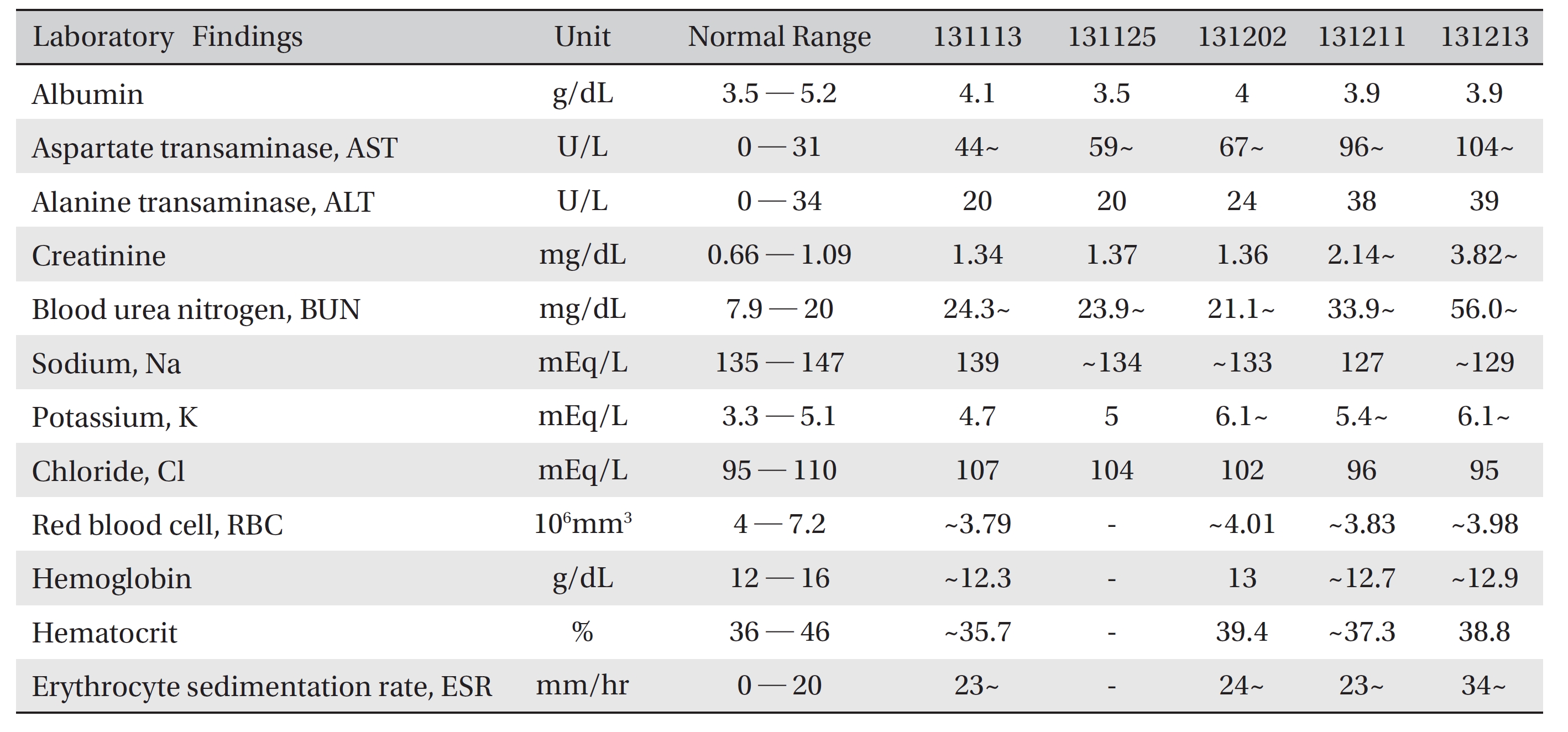
The patient was initially diagnosed with an adenocarcinoma of the lung in the right upper lobe region and received a RUL lobectomy and a RML wedge resection. After 3 years of follow-up, pleural metastases were confirmed. After taking oral anti-tumor medication for a month, the patient complained of a rash, dry skin, and diarrhea, and 5 days after admission, she also mentioned having pain in the right flank. The pain was described as an electric-shock sensation that radiated from the right flank to the inner upper right abdominal region with a VAS score as high as 7 when severe. This type of cancer pain was suspected to be caused by pleural seeding. The pain disappeared the day after her first ANP treatment. After 5 treatments of ANP, the patient was discharged from the hospital pain free (VAS score = 0). The patient was able to perform daily activities without taking any analgesics during her admission (Table 2), (Fig 3).
[Table. 2] Laboratory findings (case 2)
Laboratory findings (case 2)
This case involved an 81-year-old male patient with a weight of 58 kg and a height of 167 cm.
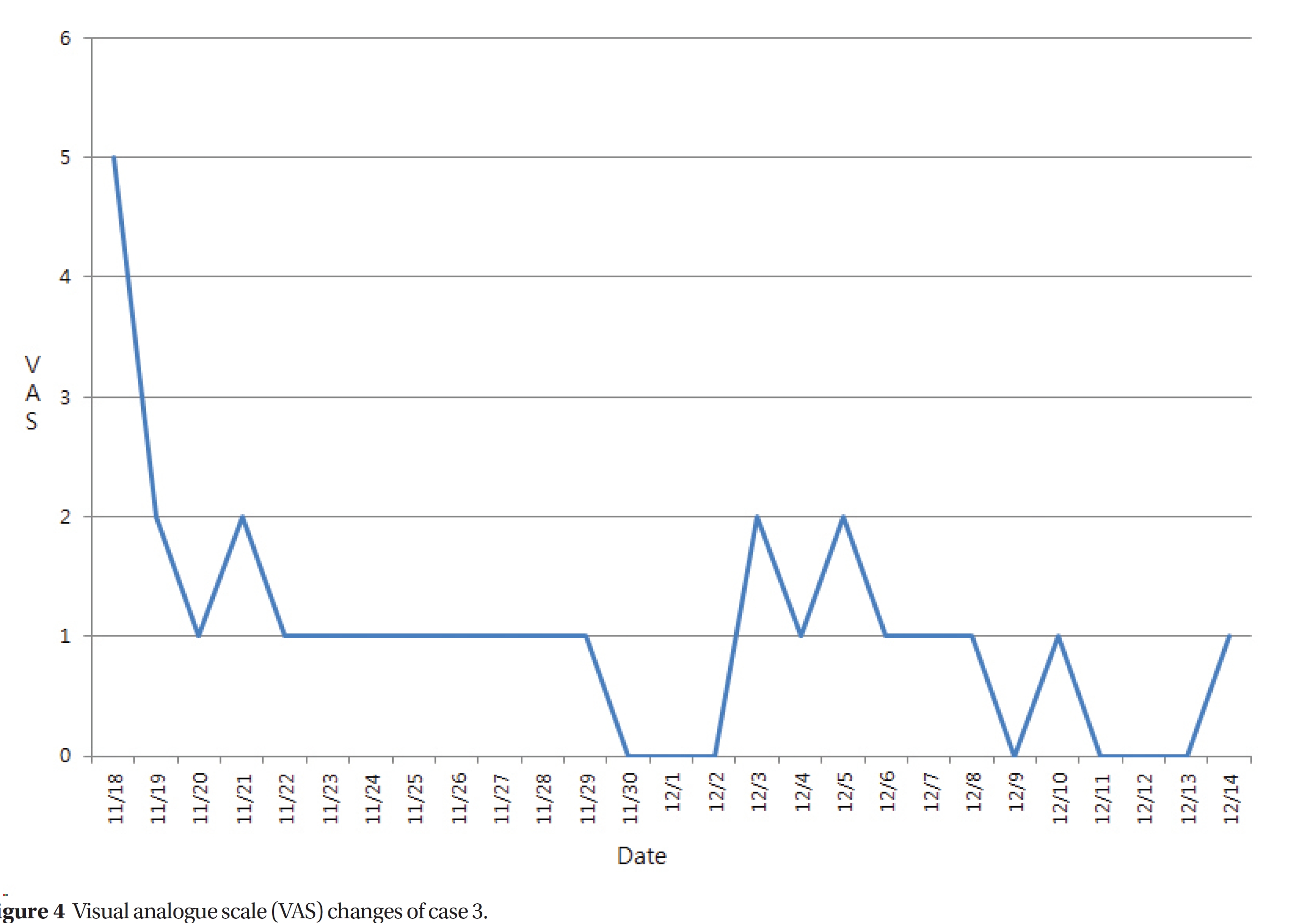
The initial diagnosis was made on October 31, 2013. The pathological diagnosis was a tubulovillous adenoma 15 cm above the anal verge, and biopsy revealed a neuroendocrine carcinoma, with the primary lesion located in the rectosigmoid colon. Initially, the parasacral lymph nodes were positive and metastasis was detected in the liver. The initial stage of the cancer was ⅣA. She had undergone neither surgery nor chemotherapy. Common complaints were diarrhea, abdominal discomfort, rash, and dyspnea. The patient was admitted from November 13, 2013, to December 14, 2013, and ANP was administered from November 18 to December 14, 2013, for a total of 13 times. The analgesics Diclofenac (2 mL, IM injection) was used as follows: 11/15/2013: at 18:00, 0.5 ample and at 24:00, 0.5 ample, 11/16/2013: at 9:00, 0.5 ample and at 20:00, 1 ample, 11/17/2013: at 10:00, 0.5 ample, 11/21/2013: at 17:00, 0.5 ample, 12/03/2013: at 17:00, 0.5 ample, and 12/11/2013: at 12:00, 0.5 ample.
This patient was admitted to the hospital with a diagnosis of a neuroendocrine tumor of the colon with multiple liver metastases. On the third day, he complained of acute right upper quadrant (RUQ) pain, but no unusual findings of the intra-peritoneal cavity were seen in the CT imaging. The ANP injections were given every day or every other day for his pain, and the VAS score was down to 1-2 on most days, with some days being pain free. After the autonomic nerve treatment, the patient’s condition was improved enough so that only a 1 mL injection of Diclofenac sodium was needed to effectively manage his sporadic pain episodes (Fig 4) Laboratory findings showed that the liver and the kidney functions were getting worse, but that was considered not to be due to drug-induced liver injury but to the natural progression of the disease (Table 3).
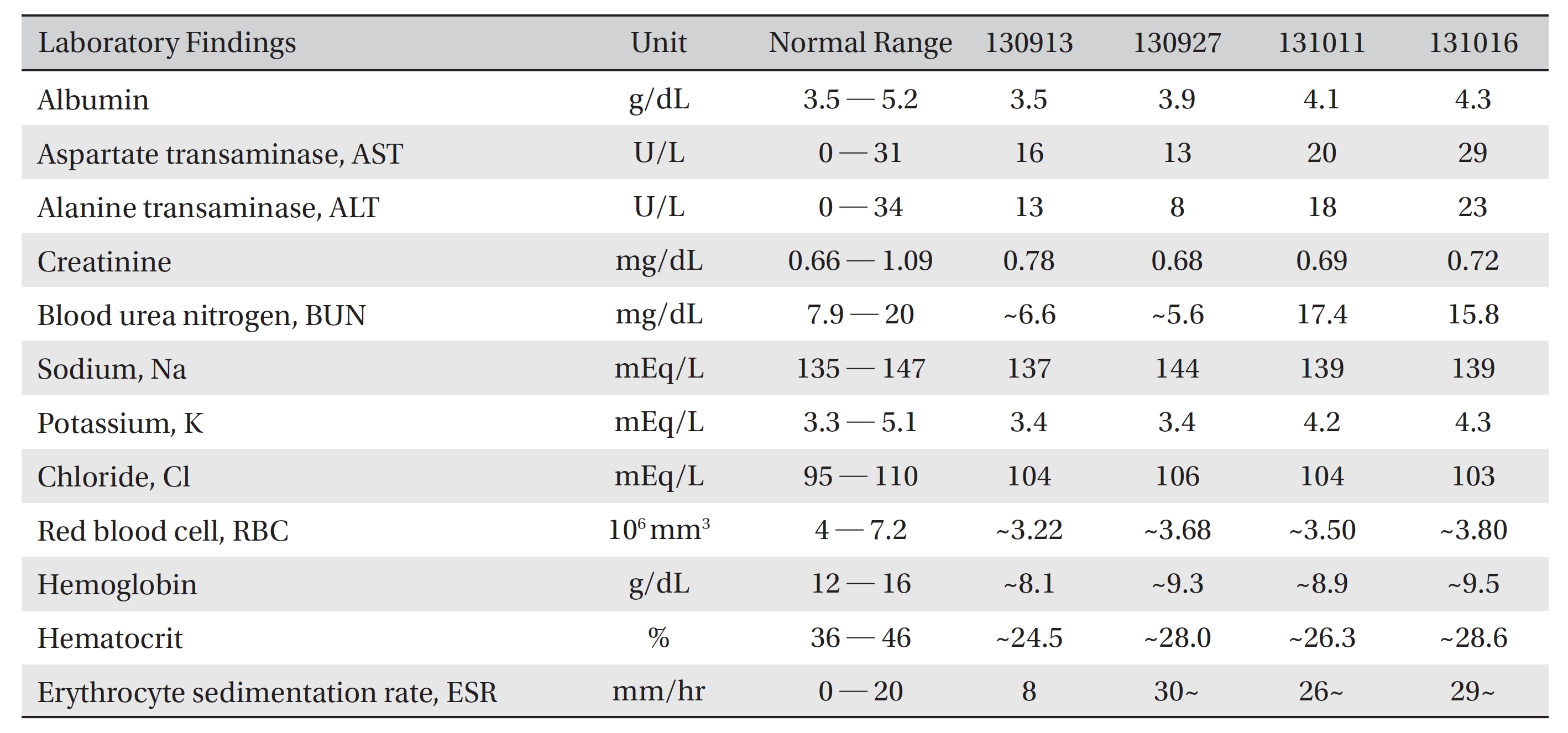
[Table. 3] Laboratory findings (case 3)
Laboratory findings (case 3)
Pain in cancer is brought on by a combination of biological, psychological and social factors [
The mechanism of acupuncture’s analgesic effect is still not clear despite its wide usage and the large amount of research. According to research on mice models, adenosine, a neuromodulator with anti-nociceptive actions, is released during acupuncture, and the expression of the adenosine A1 receptor is believed to mediate the analgesic effect of acupuncture [
Three patients with different types of advanced cancer who received ANP in this case series showed reduced degree of pain. The VAS scores of the patients decreased during the treatment period. In addition, as the treatment progressed, the analgesics dosage of two patients gradually decreased. In the study, ANP was shown to be beneficial in controlling cancer pain. Although these cases had successful outcomes, caution is needed in generalizing these results as the findings may not be transferable; further research is needed to establish the benefits of using ANP for cancer pain management.