Qigong is a form of meditative practice involving deep breathing, mental focusing, and meditation. The main effect of Qigong is to prevent and treat the disease by regulating posture, breathing, relaxation, and will concentration, management. It regulates the function of organs and builds up, and develops the powers latent within one. According to the oriental medicine theory, Qigong get meridian system to circulate and harmonize energy and blood, and increase vital basic substances, Jeong (精), Qi (氣), Sin (神). The basic material or energy of composing the body and maintaining activity for life.
The adverse effect of Qigong is reported in DSM-IV, as Chinese culture-bound syndrome, Qigong psychotic Reaction. This term is defined as an acute, timelimited episode characterized by dissociate, paranoid, and other psychotic or nonpsychotic symptoms that occur after participation in the Chinese folk health-enhancing practice of Qigong (exercise of vital energy)1). Reaction after Qigong can be divided into two. One is a natural physiologic reaction, another is a pathologic reaction. A physiologic reaction may appear in various ways according to the training method, constitution, existence disease. Mostly whole body feels comfortable, lightweight luggage, and fresh and stable. Training in a tense state, concentration by force, holding breath by force, and falling into the body shaking tend to lead to adverse reaction. When the body shaking is happened, is called oe-dong (外動), one had better disembogue than obsess. The symptoms of adverse effect of Qigong are similar to that of Qi disease. Most of symptoms are disappeared when stop the practice. But if it lasts, one should be treated.
Qigong is generally considered to be safe in most people when learned from a qualified instructor. In theory, underlying psychiatric disorders may worsen with unsupervised internal Qigong practice. The theoretical basis for this would be that an increased circulation of Qi could induce the release of repressed emotions or thoughts. Abnormal psychosomatic responses or mental disorder may be induced when Qigong is practiced inappropriately, excessively, or when practiced unguided in predisposed individuals2).
Here we reported a case of Qigong-induced Mental Disorder (QIMD). A woman who had not had a psychiatric disease, by chance started Qigong practice, and felt raising-Qi symptoms, including headache. We consider the diagnostic status of QIMD according to this case.
Ms. J is a 43-year-old female. She had worked in a community welfare center as a counselor for several years. Meanwhile, she started Enneagram study group and began to get the spirituality. And then she began to practice the Qigong in earnest, she got QIMD eventually. For that reason she had been hospitalized for 19 days. Her symptoms are quite decreased but she is currently receiving out-patient services for ongoing treatment yet.
Prior to hospitalization, she had practiced Qigong for six months. Two months ever since she started Qigong, she had unusual experiences and she felt her senses were heightened. The Qi went up and down through her back. She had a kind of feeling her garret unfurnished. But she continued Qigong running parallel with taking a walk. She practiced Qigong in earnest at a small hermitage where she stayed alone with an ascetic she called as ‘master’. She felt the master wanted her break off the relationship with a monk she had gone back, she felt the master wanted her practice harder. She often said ‘The master wanted to me∼’. But he had never said aloud, everything was her suppositions. At first that relation was okay for her, but she became felt pressure to meet the master’s expectation and gradually she was scared by him. She bore the master contradictory emotion. Then one day, She experienced a deadish fear like panic attack. She was extremely starving at that moment, and had fear of dying, feeling of detachment, and feeling of unreality. So she escaped the hermitage calling for ambulance. After that event for three months because of fear she was tired from lack of sleep. When she close her eyes, she was like dead. She feel like fall over a precipice.
When She visited our hospital, she complained of blurred vision, headache, episodic weakness, and depersonalization. She used to think about and be afraid of something that is suggestive of death. She worried for fear of losing touch. In the past, she watched drama comfortably, but nowadays watching the drama taken with shaking technique, she said it is too stamped on her memory. The skin and muscle of chest were sore. She felt sharp pains all over her body. Awake the body aches disappeared, asleep appeared.
3. Psychiatric history and previous treatment
She had not gotten any psychiatric diagnosis or treatment. She just has a sensitive character. She was rather worried about her psychiatric mental treatment record. Also, she doubted whether the treatment was going in the right direction. She thought she should be cured with Qi somewhere else not in hospital.
4. Social and developmental history
Her father was fisherman. Her mother was a woman like amazone. She didn't get a guernsey by her mother who was strict and wild. Unlike her mother, being sensitive and timid, she felt lonely and thought she was good at nothing. She was scared of mom. She had a good relationship with father. She was pretty connected with him. She understood her mom after studying Enneagram.
Her married life was smooth. She was in a settlement house, consulting for a unemployment benefits. Her husband was a computer programmer. She was a committed Buddhist. Her husband was not a Buddhist, but kind to Buddhism. She has two girls. One is in the first year of high school and the other is in the first year of middle school. Sometimes her donation for the temple cause some economic loss to home, but not serious.
There was no family psychiatric history.
During admission treatment, her anxiety gradually decreased. She had not experienced neither deadly fear nor starving feeling. But blurred vision and headache were continued daily up and down severity.
After two weeks of admission treatment, she started control her hypersensitive thoughts like ‘my breath is ascending along backbone’, ‘I feel the moment that there was no borderline myself and others’, and ‘When I was watching TV screen, it change to unreal’. She said that such thoughts were not as strong as before, and when such thoughts came up, she called ‘Stop’ inwardly, then she can control them.
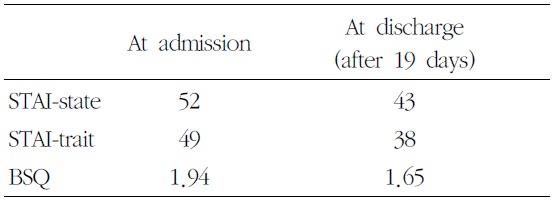
Her anxiety scales were checked up by State- Trait Anxiety Inventory (STAI), Bodily Sensations Questionnaire (BSQ). The state and trait anxiety scores were all decreased from 52 to 43, 49 to 38 respectively (Table 1).
In Pubmed searching, we found QIMD was classed as the adverse effects of breathing exercises. The ‘breathing exercises’ is a mesh term of Qigong practice.
The discussion about the adverse effect of Qigong was animated in the late 1980s and 1990s. Last the article (Shan HH, 2002), there have been no more article about QIMD.
An article (Shan HH, 1989) mentioned clinical phenomenology of mental disorders caused by Qigong exercise. One hundred and nine patients with mental disorders caused by Qigong psychophysical exercise deviation are studied. These patients were divided into schizophrenic type (47 cases) and neurotic type (62 cases). And they were analyzed by standard psychiatric rating scales and improved Minnesota multiphasic personality inventory (MMPI). The clinical characteristics could not be classified into extent psychiatric disease units. Most of these patients manifested specific physical symptoms of Qigong deviation. The authors suggest that this kind of mild, benign mental disorder associated with the unique culture be studied to contribute to the study of the classification of mental disorders. Qigong triggered disorders usually normalized during short term follow-up.
In another article (Xu SH, 1994), a series of physiological and psychological effects occur in the course of Qigong training, but inappropriate training can lead to physical and mental disturbances. Physiological effects include changes in EEG, EMG, respiratory movement, heart rate, skin potential, skin temperature and finger tip volume, sympathetic nerve function, function in stomach and intestine, metabolism, endocrine and immunity systems. Psychological effects are motor phenomena and perceptual changes: patients experienced warmness, chilliness, itching sensation in the skin, numbness, soreness, bloatedness, relaxation, tenseness, floating, dropping, enlargement or constriction of the body image, a sensation of rising to the sky, falling off, standing upside down, playing on the swing following respiration, circulation of the intrinsic Qi, electric shock, formication, during Qigong exercise. Some patients experienced dreamland illusions, unreality
[Table 1.] STAI, BSQ Before and After Admission
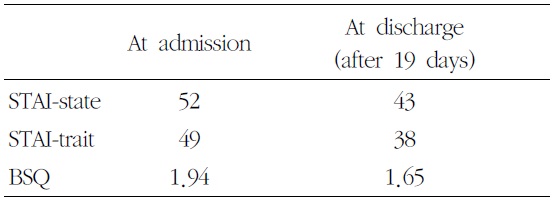
STAI, BSQ Before and After Admission
and pseudohallucination. These phenomena were transient and vanished as the exercise terminated. Qigong deviation syndrome has become a diagnostic term and is used widely in China.
In review article (Ng BY, 1999), relevant literature published in Chinese and English is reviewed. Qigong, when practiced inappropriately, may induce abnormal psychosomatic responses and even mental disorders. However, the ties between Qigong and mental disorders are manifold, and a causal relationship is difficult to establish. Many so-called 'Qigong-induced psychoses' may be more appropriately labelled 'Qigong-precipitated psychoses', where the practice of Qigong acts as a stressor in vulnerable individuals.
There was a debate about status of QIMD between Shan H. (2002) and Lee S. (2000, 2001). One insisted that Qigong induced mental disorders is an inherent disease in Chinese, another insisted that a kind of Chinese hypnosis.
The inclusion criteria for QIMD were normal behaviour before starting Qigong practice, psychophysiological reactions appearing during or after Qigong practice, manifestations of Qigong deviation syndrome not concurring with the diagnosis of schizophrenia and neurosis1).
The most frequent disorder misunderstood is somatoform disorder. The features of disease that symptoms are nonspecific and the intensity of symptom is change with patient’s condition or emotion is similar to that of Qigong-induced disorder. Nearly all patients have a special complaint of something like “the Qi moving within the body, and dashing or rushing into the head”. Often, such ‘Qi’ becomes stagnated somewhere, leading to headache, dizziness, or strange perceptions in the lo-wer abdomen1). And it was same in this case.
2. Differential diagnosis with somatoform disorder
A Somatoform disorder, is a mental disorder characterized by physical symptoms that suggest physical illness or injury- symptoms that cannot be explained fully by a general medical condition, direct effect of a substance, or attributable to another mental disorder3). The symptoms that result from a somatoform disorder are due to mental factors. In people who have a somatoform disorder, medical test results are either normal or do not explain the person's symptoms. Patients with this disorder often become worried about their health because the doctors are unable to find a cause for their health problems. But above all she was applicable to none of somatoform disorder group, conversion disorder, somatization disorder, hypochondriasis, body dysmorphic disorder, and pain disorder. Thinking undifferentiated somatoform disorder, the most frequent form of somatoform disorder4), she did not have a specific mental factor and so worry about her health. It is against the major feature of somatoform disorder.
3. Differential diagnosis with schizophrenia
Schizophrenia is a mental disorder characterized by a disintegration of thought processes and of emotional responsiveness5). It most commonly manifests as auditory hallucinations, paranoid or bizarre delusions, or disorganized speech and thinking, and it is accompanied by significant social or occupational dysfunction. Diagnosis is based on observed behavior and the patient's reported experiences. But she did not appear any of auditory hallucinations, paranoid or bizarre delusions, or disorganized speech and thinking. Her body sensations and thoughts about Qi were a little bit bizarre, but it was not as much as she lost her reality.
Delusions (“non-bizarre”) are also present in delusional disorder, and social withdrawal in social anxiety disorder, avoidant personality disorder and schizotypal personality disorder. But none of them were not relevant her.
4. As an independent disease, QIMD
As mentioned above QIMD does not come under current somatoform disorder subtypes and schizophrenia. It has distinct characters that occurring after Qigong practice, symptoms of upper body, feeling that something to rise up.
Nowadays more and more people are practicing Qigong, not limited to eastern Asia. Moreover recent researches are focusing on how each composition factor of Qigong effect on specific disease6,7). So how Qigong act on healthy people and induce which aspect of psychiatric symptoms should be actively studied.
There was one report about documents erratic blood pressure elevation in this patient while she was practising Qigong. They thus recommend that persons wishing to practise Qigong have a general body and blood pressure check before embarking on this, or any other form, of vigorous exercise8). The diverse adverse effects and curative effects should be accrued.