Osteoarthritis (OA) is a degenerative joint disorder characterized by progressive cartilage damage and loss, changes in bone and other periarticular tissues, and commonly, secondary joint inflammation [1]. Osteoarthritis of the knee represents approximately 40~60% of musculoskeletal disease and is the most common form of OA, with a huge socioeconomic and healthcare burden [2,3]. Because knee OA is a chronic and progressive disease, pain control or pain management is difficult [4]. Recently, the number of people who are affected by degenerative diseases has increased, especially among an increasing aging population, so a multifaceted approach for the treatment of degenerative knee arthritis is required.
In Oriental medicine, acupuncture and moxibustion treatment, herbal medicine, pharmacopuncture treatment, etc. are used to treat knee OA. Acupuncture is a very popular treatment for OA in many Asian countries, and its popularity is increasing in western countries. Systematic reviews and randomized controlled trials support the effectiveness of acupuncture for the treatment of OA pain [5,6]. Among the treatments, pharmacopuncture treatment is a new form of acupuncture treatment combining acupuncture and herbal medicine [7,8]. In recent pharmacopuncture treatment especially, bee venom pharmacopuncture (BVP) has been widely used.
Many studies have been performed on BVP and have demonstrated significant efficacy for the treatment of knee OA [9-15]. Existing treatment methods for using BVP to treat knee OA are intradermal, subcutaneous, intra-acupoint, and intra-articular injections, etc. [16].
Previous studies on treatment methods for applying bee venom to treat knee OA have had limitations, including parallels to other treatments and the absence of a control group, and no direct comparative studies among methods of treatment have been conducted. [9-15]. Thus, randomized controlled trials on treatment methods are needed. The aim of this study is to compare intra-acupoint injection, intra-articular injection, and intra-acupoint injection combined with intra-articular injection with BVP and to analyze the efficacy of each for the treatment of knee OA.
Sixty-nine patients were recruited by the Department of Acupuncture and Moxibustion at Dong-Eui Oriental University Hospital from February 1 to July 23, 2012. Inclusion criteria included an age of at least 40 years but below 80 years, presence of knee OA diagnosed by an orthopedist based on the American College of Rheumatology classification criteria, knee pain in one or both knees rated ≥ 4 on the Visual Analog Scale (VAS).If they have used medications for osteoarthritis but hasn't changed medication during the past month and treatment began after had been stopped medication for one week. Exclusion criteria included prior artificial joint surgery, history of prolotherapy, injection of hyaluronic acid or use of cortisone within the last 3 months, serious organic disease, including mental disorders and autoimmune disease, use of nonsteroidal anti-inflammatory and adrenal cortex hormone medicines for other diseases, post-traumatic degenerative arthritis, history of skin irritation, and severe problems of the cardiovascular, lung, liver, kidney or hematopoietic systems or other serious primary diseases, cancer, and neurological joint pain.
After a brief telephone screening, participants were asked to visit the hospital for a demographic survey examination, a history of disease duration, a consent statement, physical examination and a knee X-ray. Subsequently, after the safety from allergic responses to bee venom had been ensured, the first treatment was administered.
The purpose of this study is to compare the effects of BVP therapy according to the treatment methods for three groups: BVP injection at intra-acupoints combined with intra-articular injection (experimental group); BVP injection at intra-acupoints (control group Ⅰ); and BVP intra-articular injection (control group Ⅱ). The partici-pants were assigned in the order in which they were recruited.
To identify bee venom hypersensitivity in all the groups, we injected 0.05 ml of BVP at 1:10,000 which was diluted with BVP1:4000 (Korean Pharmacopuncture Institute) and 5% dextrose solution (Choongwae Pharma Co., Seoul, Korea) on intradermal of LI11 (Quchi) by using 1-ml 8-mm 30-guage syringes (Shin Chang medical, Co. Ltd.). After 15- 20 minutes, at the peak of redness, we considered swelling of more than 5 mm in diameter and a rash of more than 11 mm as positive. For negative indications, we performed the following procedure: For the experimental group, 0.1 ml of BVP (1:10,000) was divided into ST35 (Dubi), GB34 (Yanglingquan), EX32 (Xiyan), ST36 (Zusan Li), and SP9 (Yinlingquan) on the affected side (one side or both sides) by using 1-ml 8-mm 30-guage syringes. The depth of needle insertion was about 3-5 mm. The treatment amount was increased by 0.1 ml each time. If necessary, ashi acupoints were injected.
The method of intra-articular injection was as follows: Participants were in the supine position with their legs stretched out. The patella was pushed to the medial direction so that the knee joint cavity could be opened. BVP (0.1 ml at 1:10,000) was injected obliquely (laterally and slightly posterior) into the medial inferior border of the central patella with a 1-ml 25.7-mm 27-guage syringe (Shin Chang Medical. Co. Ltd.). The treatment amount was increased by 0.1 ml each time.
For control groupⅠ, the method was the same as that used for the experimental group (acupoints and injection method) BVP (0.2 ml at 1:10,000) was injected. The treatment amount was increased by 0.2 ml each time. For control groupⅡ, BVP (0.2 ml at 1:10,000) was injected into the knee joint cavity by using the same method as that used for the experimental group. The treatment amount was increased by 0.2 ml each time. After the injection, parti-cipants exercised flexion and extension of the knee joints 3-5 times to spread the solution evenly in the knee joint cavity. The amount of bee venom for a treatment was a maximum of 1 ml in all groups. Treatments were done twice a week, for a total of 9 times. If participants showed hypersensitivity reactions but did not drop out, the amount of the scheduled injection was reduced by half, but the concentration was increased to 1:5000; therefore, the amount of bee venom was maintained, or the participants were injected with bee venom 3-5 days later than the scheduled time.
The VAS (score range: 0-10 cm) was used as the primary outcome measurement [17]. For bilateral OA participants, the side with more pain at baseline was evaluated throughout the study:before the 1st treatment (V1), before the 3rd treatment (V2), before the 5th treatment (V3), before the 7th treatment (V4), before the 9th treatment (V5), and 4 weeks from the 9th treatment (V6), for a total of six evaluation. The Secondary outcome measurement was a patient global assessment of the change in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC, Likert scale version; score range: 0-96) [18]. The total WOMAC score was a summation of the scores for each individual domain: pain (score range: 0-20), stiffness (score range: 0-8), and physical function (score range: 0-68). The Korean version of WOMAC was used in this trial [19], before the 1st treatment (W1), before the 5th treatment (W2), before the 9th treatment (W3), and 4 weeks after the 9th treatment (W4), for a total of four evaluatio-ns. X-ray examinations were done at Orthopedic Surgery Department at Dong-Eui Medical Center before treatme-nt, to show the degree of regression on the Kellgren-
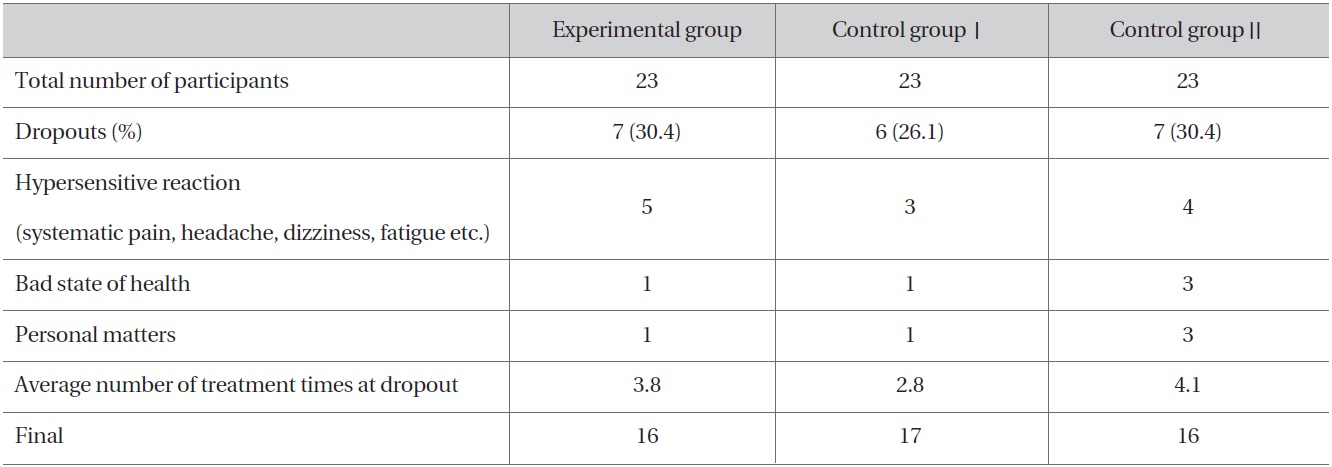
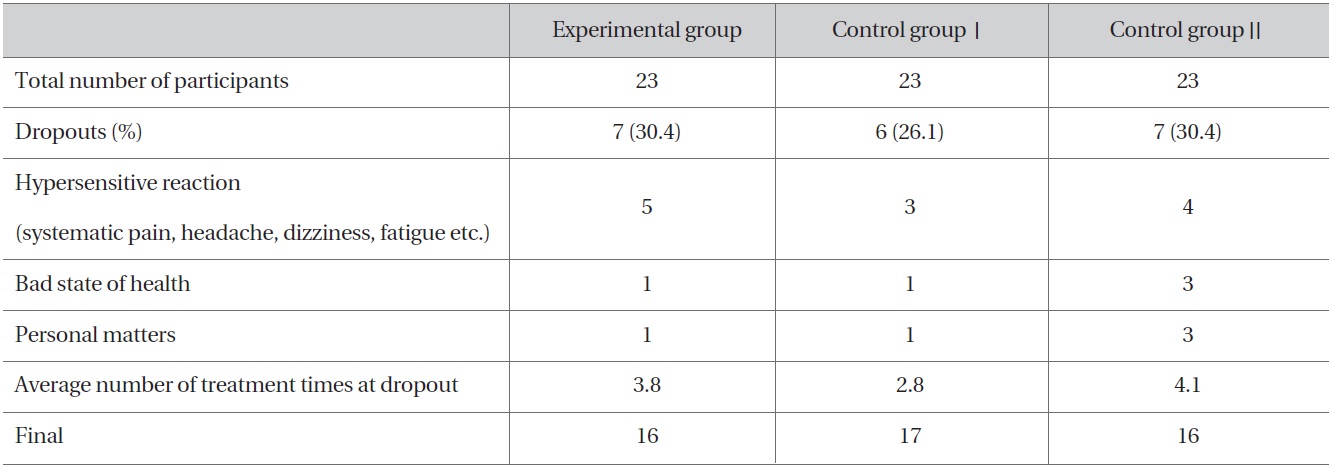
Analysis of dropout
Lawrence scale (K-L score). A statistical analysis with SPSS 18.0 for Window was used. We evaluated for the baseline characteristics of the groups by using the chi-square test and the one-way ANOVA. Statistical differences of improvement in each group were evaluated by using the paired
Table 1 shows analysis of dropout in the three groups. Except for dropouts for personal reasons, the average number of treatment times at dropout due solely to hypersensitivity reactions was 3.5 in the experimental group, 2.8 in control groupⅠand 4.5 in control groupⅡ.
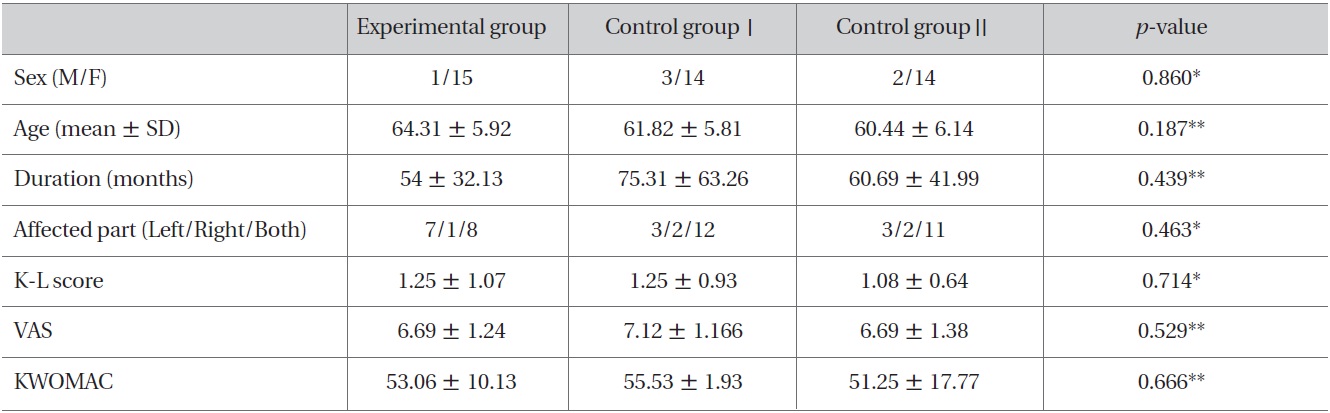
Fourty-nine participants were between 49 and 74 years old, and 93% were women. Table 2 shows general characteristics and the baseline VAS and KWOMAC scores for the three groups. No significant differences in demographic characteristics or baseline VAS and KWOMAC scores were observed among the groups (Table 2).
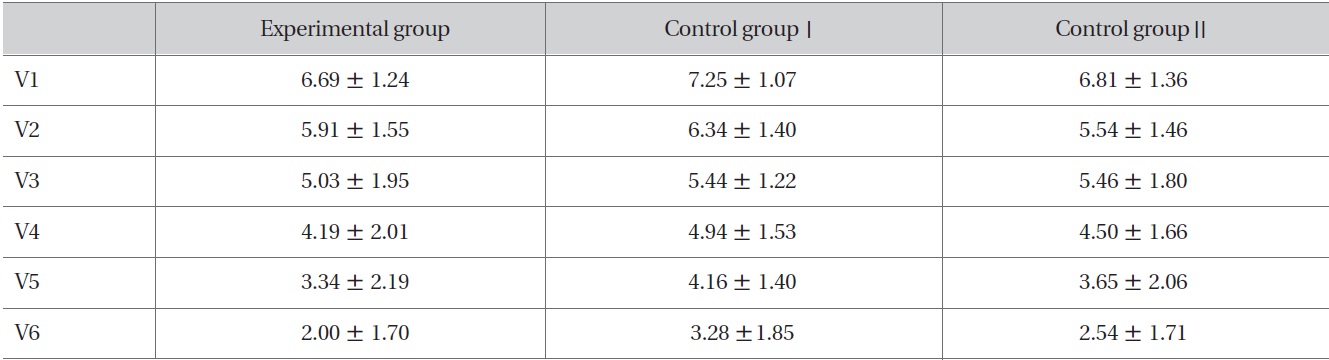
In all three groups, the changes after checking the VAS scores six times are shown in Table 3. Compared to V1, significant improvement was shown after V2 (Table 4). Also, significant improvement was shown according to the progress of the treatment (experimental group: F = 22.924,
All three groups also showed improvement in the four-week follow-up after the trial had ended. The three groups showed no significant differences in improvement at each stage, but the order of the level of improvement of the
[Table 2] Baseline characteristics of participants.
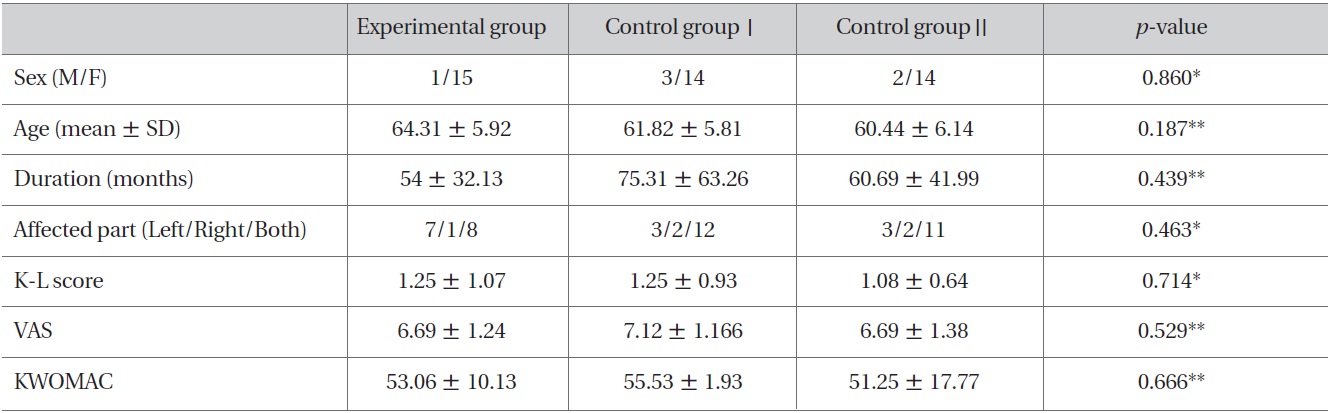
Baseline characteristics of participants.
[Table 3] Change of VAS in each group.
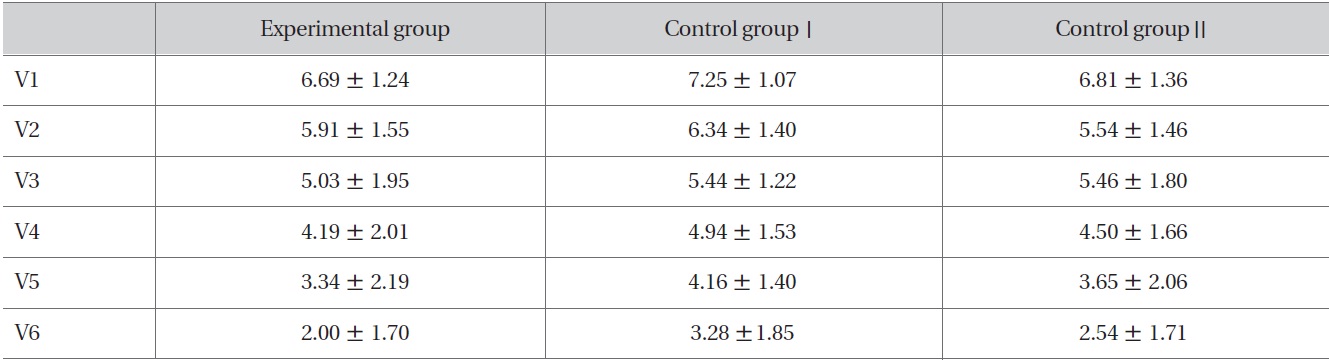
Change of VAS in each group.
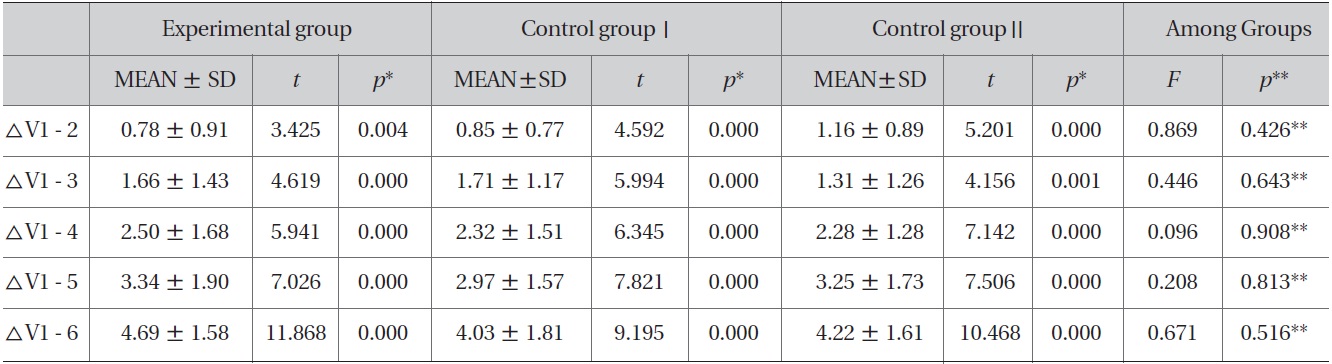
[Table 4] Improvement of VAS in each group and comparison of improvement among groups
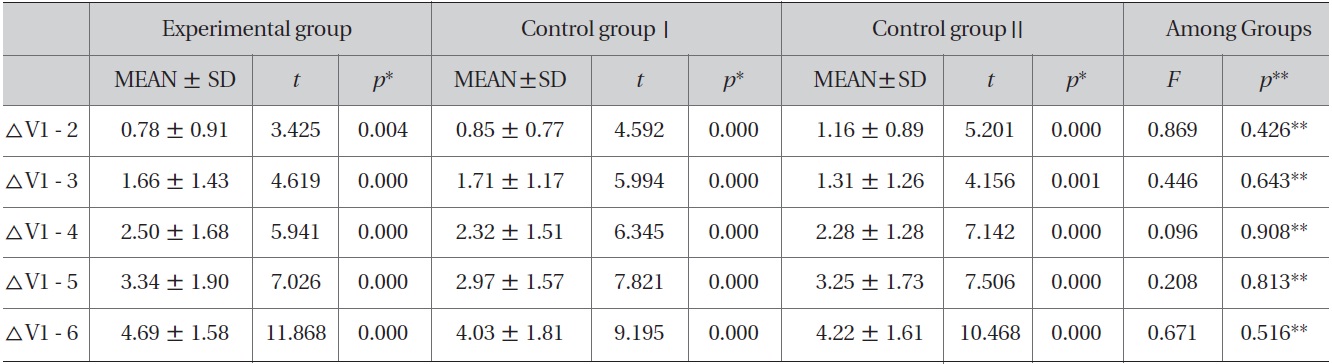
Improvement of VAS in each group and comparison of improvement among groups
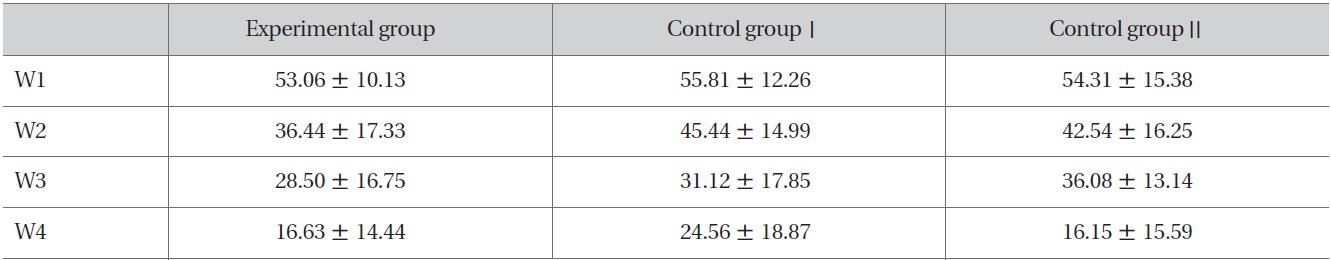
[Table 5] Change of KWOMAC in each group
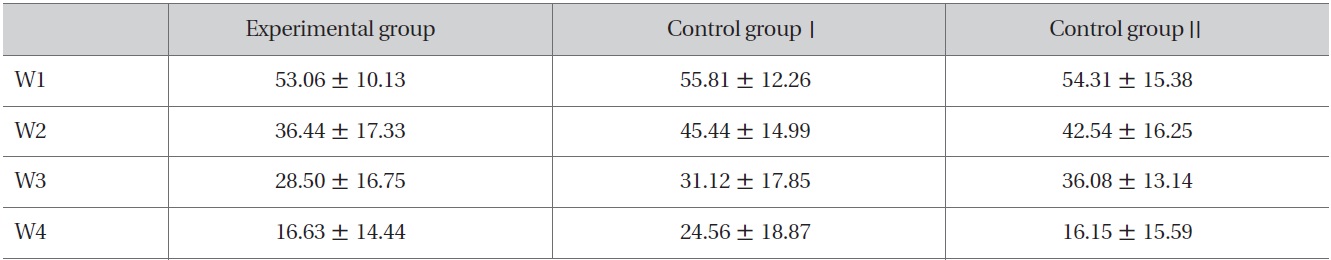
Change of KWOMAC in each group
[Table 6] Improvement of KWOMAC in each group and comparison of KWOMAC among groups
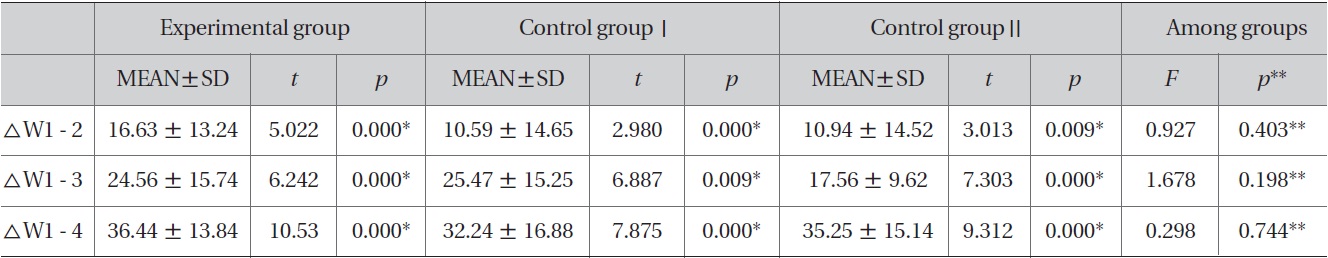
Improvement of KWOMAC in each group and comparison of KWOMAC among groups
groups was the experimental group, control group Ⅱ, and control groupⅠ at the end of the trial, and at the four week follow-up after the trial ended (Table 4).
In all three groups, the changes after checking the KWOMAC score four times are shown in Table 5. Comp-ared to W1, significant improvement was shown after W2 (Table 6). Also, significant improvement was shown according to the progress of the treatment (experimental group : F = 40.141 ;
Knee OA has been recognized as a 'Bi' syndrome or 'Haksulpoong' in Oriental medicine [20].
BVP is prepared with bee venom from live honey bees and is artificially extracted and refined [21]. It has varying actions on the immune system, anti-inflammatory and analgesic actions, cell lysis, neurotoxic and antibacterial actions, antipyretics, and invigoration of blood circulation. Therefore, it can be used for a wide range of diseases, including acute chronic arthritis, muscle pain, neuralgia, gout, etc. [22,23].
BVP should be used carefully in treatment because allergic reactions are stronger than they are for other pharmacopunctures due to a combination of the antigens of the heterologous proteins and antibody. Therefore, because a stabilization of the body's immune system to bee venom is needed, in this triala small dose of BVP was used at first and was then increased gradually [24]. Existing treatment methods for using BVP to treat knee OA are intradermal, subcutaneous, intra-acupoint, and intra-articular injections, etc.
With intradermal injection, the response of the body after treatment can be identified precisely, and hyper stimulation and side effects can be controlled quickly. However, it has the disadvantage of severe skin pain and itching. With subcutaneous injection, treatment is quick, and pain and itching are reduced. However, identifying the response of the body after bee venom injection is difficult, and a risk of injecting bee venom into a blood vessel exists [16]. With intra-acupoint injection, absorption of bee venom is faster than it is intradermal or subcutaneous injection and injection painis reduced [7]. With intra-articular injection, treatment takes less time, and systemic hypersensitivity is relatively reduced. However, identifying the body's response after bee venom injection is difficult and incorrect injection can cause severe pain [16].
In reviewing previous studies on the treatment method for using BVP to treat knee OA, Lee and by An et al. [9,12] reported that intradermal BVP injection was significantly more effective than filiform acupuncture. A study by Kim et al.[14] reported that intramuscular injection had no significant difference compared with intradermal injection, but did have more effect. A study by Rye et al. [15] reported that intra-articular BVP injection was significantly more effective than filiform acupuncture.
In this study we tried to compare intra-acupoint injection, intra-articular injection, intra-acupoint combined with intra-articular injection with BVP and to analyze the efficacy of these treatments for knee OA. We excepted intra-dermal injection which is widely used because the progress of clinical trials might be difficult due to the increased number of control groups. The acupoints used were ST35, GB34, EX32, ST36, and SP9 because Kim et al. concluded that these acupoints were effective for treating Knee OA through an analysis of 21 RCT papers [25].
Approximately 12 (22%) of all participants had allergic reactions to the procedure. These hypersensitivity reactions caused discomfort to the patient or the practitioner. Despite the excellent effects of BVP, the reactions cause practitioners to tend to avoid using BVP in clinics [10]. Control groupⅠhad the highest numbers of dropouts due to hypersensitivity reactions and the lowest average number of treatment times at dropout. On the contrary, control groupⅡhad the lowest numbers of dropouts and the average number of treatment times at drop out was the highest. However, there were no significant differences.
The reason for these results seemed to be that the risk of hypersensitivity reactions was relatively infrequent for intra-articular injection which injects BVP on points isolated from systemic circulation [16]. However, in the case of intra-articular injection, some patients complained of severe stiffness due to edema. During this trial, if participants showed a certain degree of hypersensitivity reactions or participants wanted to continue treatment in spite of hypersensitivity reactions, the amount of the scheduled injection was reduced by half, but the concentration was increased to 1:5000. Therefore, the amount of bee venom was maintained because the effects of bee venom treatment are not related to the volume of the injected BVP, but to the amounts of the bee venom ingredients [16]. The intent was to decrease the discomfort of the patient by reducing the volume of BVP injected while maintaining the amounts of bee venom ingredients. Especially in the case of edema, reducing the volume of the BVP injected may relatively decrease the discomfort of the patient.
The results showed that all three groups experienced significant changes in the VAS and the KWOMAC at the 1 - week assessment and according to the progress of the treatment. Moreover, the four-week follow-up after the final treatment showed a persistence of BVP effects. However, when the groups were compared, no statistically significant difference in the VAS and the KWOMAC were noted.
In comparing the effects among groups after the final treatment and at the four-week follow-up after the final treatment, the VAS was not consistent with the KWOMAC pattern due to the subjective assessment of the participants own pain with the VAS, and the KWOMAC being composed of sub-items of pain, stiffness, and function. In addition, the pain KWOMAC score was not consistent with the VAS pattern because the results were estimated from a KWOMAC questionnaire which might have been difficult for most elderly participants to complete.
In this study, the results showed that intra-articular injection was more effective than intra-acupoint injection. Especially intra-acupoint combined with intra-articular injection was the most effective among the three treatments. A study by Ryu et al. [15] reported that intra-articular injections for treating knee OA was more effective in reducing pain and improving joint function; consequently, a rapid analgesic effect can be achieved with this treatment method. Intra-articular injection inserted bee venom closer to the affected lesion compared with subcutaneous injection. By pharmacokinetics, the drug injected subcutaneously acts through the circulatory system of the body via the blood vessels in the subcutaneous layers, but the drug injected intra-articularly acts locally and can increase a localized treatment effect, minimizing systemic hypersensitivity reactions or risks of side effects due to bee venom [26].
In summary, accurate intra-articular injection of BVP may be a proper treatment method for the treatment of knee OA as long as the practitioner is cautious in maintaining sterile conditions in preparing for injection to avoid infection and in managing edema properly. Moreover, combining intra-acupoint with intra-articular injection properly, depending on the patient's symptoms, may produce better results when conservatively treating knee OA. The limitations of this study were as follows: the completion of the questionnaire was difficult for elderly participants; limited concentration and capacity were used without considering the severity of the symptoms; there were relatively few participants; no detailed investigation regarding hypersensitivity reactions was done.
Thus, further studies are required to investigate the treatment methods of BVP on various body parts affected by arthritis, so that three methods can be used more aggressively in clinics.