In Korea, herbal medicine has long been used for health as well as for treatment. With increased use of herbal medic-ine, more systematic verification of its safety and effectiven-ess is now required; particularly, much controversy exists over its side effects. Studies on Korean herbal medicine use and abnormal liver function tests have been conducted as case reports [1-5], a comparative study on the result of abn-ormal liver function test before and after taking herbal medicine [6], and a study on the causes of drug-induced injury of the liver [7]. In the domestic medical world, we have a case report that herbal medicine and medicinal herbs are causes of liver injury [1], a report that they are major causes of toxic hepatitis [8,9], and a research report that herbal me-dicine is significant cause of all drug-induced liver injury [10]. On the other hand, in the world of herbal medicine, ma-ny clinical researchers have reported, based on compariso-ns of the results of abnormal liver tests before and after taking herbal medicine, that herbal medicine is rarely the cause of liver injury [11, 12], and case reports [2-5] continue to be published that Korean herbal medicine is effective for the treatment of liver disorder. Studies on foreign, there is a conflict exists between the view that the use of herbal medicine will affect the liver function [13] and the view that the use of herbal medicine will not affect the liver function [14, 15].
However, safety verification still exists in that Korean herb-al medicine is largely used in combination therapies; comp-ared to western medicine in which a single pill is extracted or produced, in korean herbal medicine, few kinds of herbs are used under the same name of medicinal ingredient, and various kinds of medicinal herbs are used for the same disease according to the diagnosis of disease symptom. In prescriptions, it is unclear whether the kinds and the compone-nts of Korean herbal medicine are revealed or the mechanisms are clear, so evaluating the impact on liver function and finding causes of liver injury is difficult [16], In case of folk medicine in which practitioners use health foods containing medicinal herbs or a single medicinal herb, those medicinal herbs are often misused without a herb doctor's prescription and guidance, and many studies on medicinal herbs, in the medicinal world which lack professional knowledge in oriental medicine and controv-ersial, have been reported.
In reality, there is a strong prejudice in our domestic medical world that the use of Korean herbal medicine may cause abno-rmal liver function, and even in herbal/western combination medicine, from time to time, those patients who took herbal medicine were diagnosed with abnormal liver function after tests. In such cases, the abnormal liver function was thought to be a side effect from the use of herbal medicine, so in most cas-es, Further use of that medicine was prohibited. In spite of this,herbal medicine continues to be used if it is considered a proper prescription, Oriental medical clinics and/or traditional herbal medicine clinics prescribe it for abnormal liver function, and when oriental herbs are administered clinically by professionals for proper disease symptoms, there are few side effects.
Accordingly, the authors made a chart and analyzed it to check the safety of herbal medicine in those patients who were hospit-alized with the diagnosis of early neuropathy and other major symptoms, but their alanine aminotransferase (ALT) was incre-ased in a blood test. They were classified the patients into a her-bal medicine group, a western medicine group, and a herbal/western combination medicine group, and analyzed the impact of continuous use of herbal medicine on patients whose liver fu-nctions showed hepatosis in tests on liver function screening. Finally, the data for the single herbal/western medicine groups and the combination medicine group were compared and signi-ficant findings were noted.
2.1.1. Inclusion criteria
A retrospective study was conducted by randomly selecting patients who were hospitalized at the Korean Herb Medicine Hospital, Dong-Eui University, from January 2011 to August 2011 and showed an abnormal liver function on a biochemical serum test among the patients who were under treatment for diseases of the nervous system. The selected patients were cla-ssified into three groups: a group of patients (30 individuals) who took herbal medicine that continued to be modified in the tradi-tional herbal medicine ward during their hospitalization after they had been diagnosed with abnormal ALT a group of patients (30 individuals) who took western medicine (i.e, medication for liver disorder) in combination with herbal medicine and a group of patients (30 individuals) who took western medication for liver disorder as a major medication because of the increased ALT in the western medicine ward. All patients were tested before and after taking the medication.
2.1.2. Exclusion Criteria
Those patients who were diagnosed with abnormal function on other tests, except the liver function test, who had a history of liver disorder/hepatitis or had been hospitalized for such a dise-ase, or who had had a previous illness because of drinking, tra-nsfusion or other underlying diseases were excluded.
Four items, aspartic aminotransferase (AST), alanine amino-transferase (ALT), alkaline phosphatase (ALP) and total bilirubin (T-bil) were investigated in the blood tests of patients who did a blood test in the blood-examination room during hospitalization. Those patients whose results deviated from the normal range were randomly selected and classified into a group of patients who only took herbal medicine in the herbal medicine ward, a group of patients who took herbal/western combination medic-ine, and a group of patients who took western medicine in the western medicine ward and did an additional test. Patients' charts were analyzed, and the results before and after blood tests were compared.
2.2.1. Herbal medicine treatment
For treatment, patients were classified according to their ma-jor disease and secondarily according to the leveling ALT. Radix puerariae lobatae (galguen), Herba artemisiae scopariae (injin), Radix bupleuri (siho), and other herbs were modified in its acco-unt. For administration, two quires of oriental medicine were administered three times a day.
2.2.2. Western medicine treatment
Capsules of Godex CAP and Legalon 140-mg CAP, which are normally prescribed with a diagnosis of abnormal liver function, except for major diseases, at the department of Neurology and Rehabilitation Medical Treatment in this hospital was adminis-tered three times a day.
2.2.3. Herbal/western combination treatment
Two quires of herbal medicine were administered to patients three times a day according to the patients’ major diseases, and capsules of Godex CAP and Legalon 140-mg CAP, were also administered at the same time a day for abnormal liver function at the Department of Neurology and Rehabilitation Medical Treatment.
2.2.4. Valuation criteria
The criteria for AST, ALT, ALP, and T-bil, were the standard criteria for blood tests at the hospital: AST 8∼35 (U/L), ALT 5∼35 (U/L), ALP 30∼120 (U/L), and T-bil 0.3∼1.3 (mg/dL), respec-tively.
SPSS 18.0K for windows was used for statistics, and the chan-ges between the three groups are shown with mean ± standard deviation. An independent
3.1. General characteristics of objects
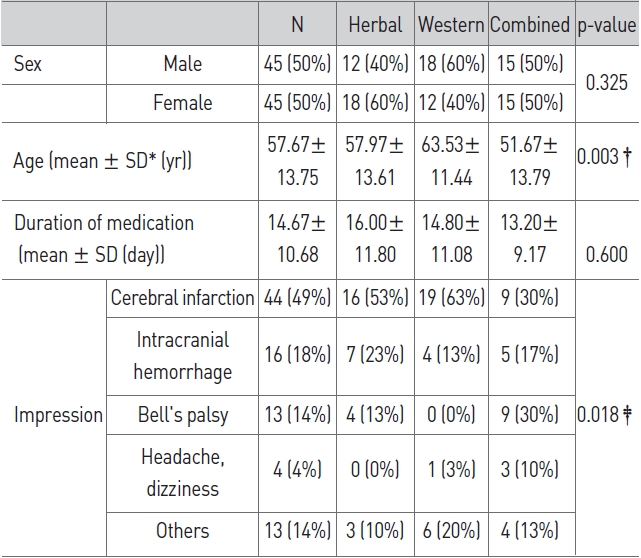
The subjects included a total of 90 patients: 45 males and 45 females. Their mean age was 57.67±13.75 years old, and the mean period of treated was 14.67±10.68 days. For Major diseases, were cerebral infarction in 44 individuals, hemorrhage in the brain in 16, facial paralysis in 13, headache and dizziness in 4, and other symptoms in 13. Twelve (12) males and 18 fema-les mean age 57.97±13.61 years old and period of treatment 16.00±11.80 days, were in the herbal medicine group; 18 males and 12 females, mean age 63.53±11.44 years old, period of treatment14.80±11.08 days, were in the western medicine group; 15 males and 15 females, mean age 51.67±13.79 years old and period of treatment 13.20±9.17 days, were in the herbal/western combination medicine group (Table 1). In the comparison of the three groups, age showed a significant difference (p < 0.01) between the herbal combined medicine gr-oup and the western medicine group, but no significant difference in the other groups. The period of treatment showed no significant difference between the three groups.
[Table 1] General characteristics of all cases
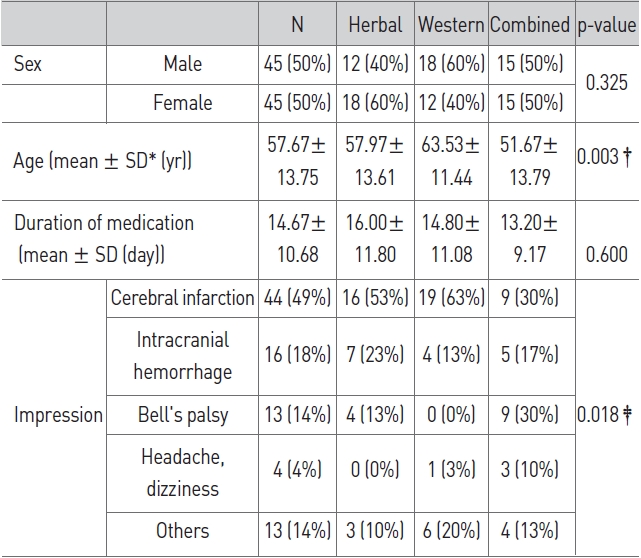
General characteristics of all cases
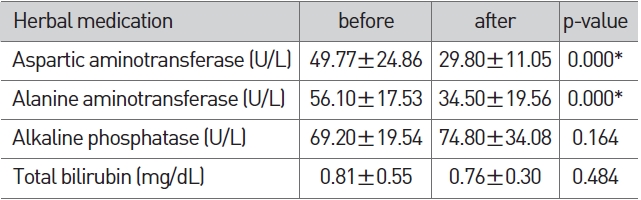
3.2. Change of LFT in the group of herbal medicine
In the herbal medicine group, AST and ALT after the admin-istration of herbal medicine showed a significant reduction (p < 0.01) compared to AST and ALT before administration of herbal medicine (Table 2).
[Table 2] Change of LFT in herbal medication
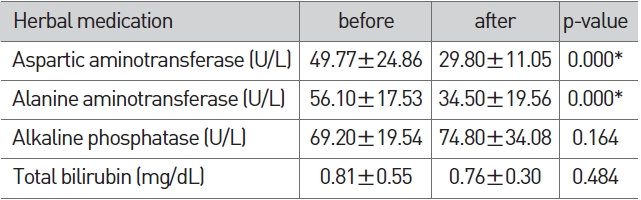
Change of LFT in herbal medication
3.3. Change of LFT in the group of western medicine
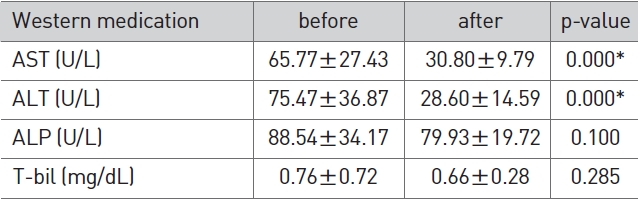
[Table 3] Change of LFT in western medication
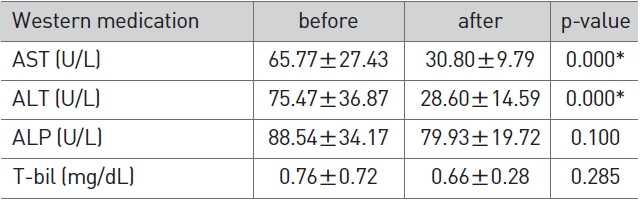
Change of LFT in western medication
In the western medicine group, AST and ALT after the admini-stration of western medicine showed a significant reduction (p < 0.01) compared to AST and ALT before the administration of western medicine (Table 3).
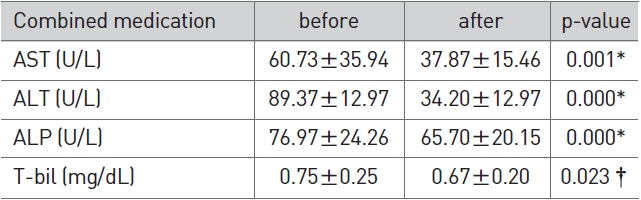
3.4. Change of LFT in the group of herbal/western combined medicine
In the herbal/western combined medicine group, AST, ALT, and ALP after combined administration showed a significant reduction (p < 0.01) compared to AST, ALT, and ALP before com-bined treatment (Table 4).
[Table 4] Change of LFT in combined medication
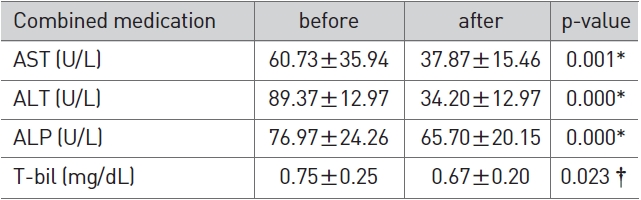
Change of LFT in combined medication
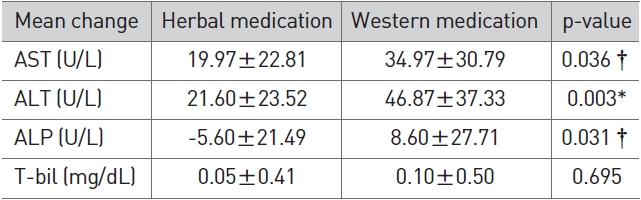
3.5. LFT Changes between the herbal medicine grou-p and western medicine group
In terms of LFT changes, the western medicine group showed a more significant reduction in AST (p < 0.05), ALT (p < 0.01), and ALP (p < 0.05) than the herbal medicine group (Table 5).
[Table 5] Comparison of LFT Changes between herbal medication and western medication
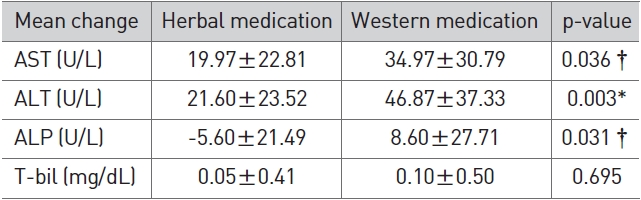
Comparison of LFT Changes between herbal medication and western medication
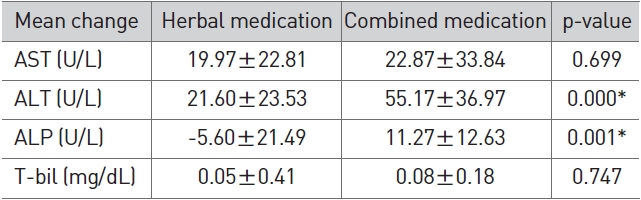
3.6. LFT Changes between herbal medicine group and herbal/western combined medicine group
In terms of LFT changes, the herbal/western combined medi-cine group showed a more significant reduction in ALT (p < 0.01) and ALP (p < 0.01) than the herbal medicine group (Table 6).
[Table 6] Comparison of LFT changes between herbal medication and combined medication
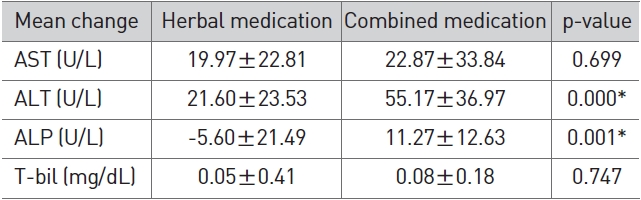
Comparison of LFT changes between herbal medication and combined medication
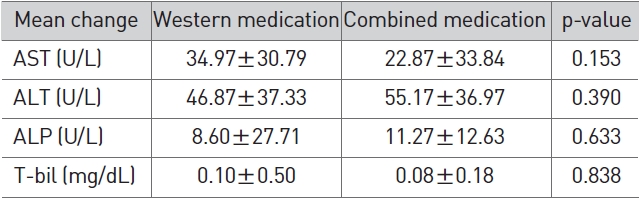
3.7. LFT Changes between western medicine group and herbal/western combined medicine group
In terms of LFT changes, no significant difference was noted between the herbal/western combined medicine group and the western medicine group (Table 7).
[Table 7] Comparison of LFT changes between western medication and combined medication
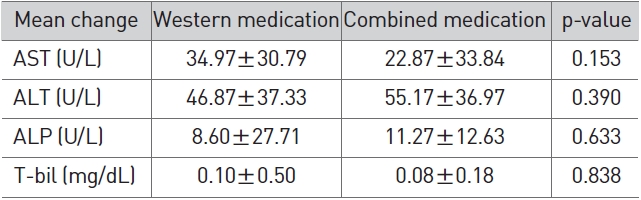
Comparison of LFT changes between western medication and combined medication
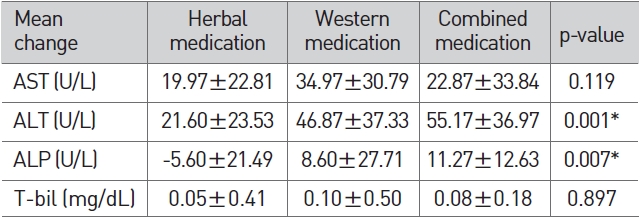
In terms of LFT changes between the three groups, AST and T-bil showed no significant difference between the three groups, but for ALT and ALP, the p-value was less than 0.05 as a result of variance analysis, and the mean values differed according to the group. Thus for ALT and ALP, which showed significant results, a post-hoc test was conducted by using theTurkeyHSD method. As a result, no significant difference was found between the western medicine group and herbal/western combined medicine group, but a significant difference was found between those two groups and the herbal medicine group (Table 8).
[Table 8] Comparison of LFT changes
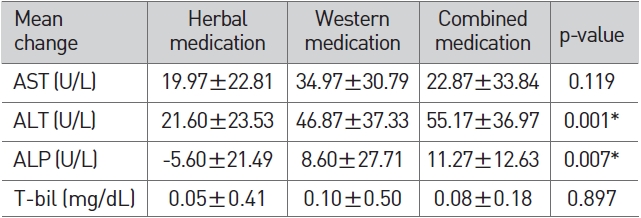
Comparison of LFT changes
Locally and abroad, the use of herbal medicine and crude dru-gs is increasing, and accordingly, there are increased reports on their side effects. In particular, liver injury caused by herbal medicine is now the subject of controversy, and herbal medicine accounts for a considerable proportion of drug-induced liver injuries, being the cause of liver injury in 29.5% of the cases [17]. In addition liver injury by herbal medicine is the cause of toxic hepatitis [9]. According to the literature published in Korea, western medicine accounts for 15.8%∼83.3% and herbal medi-cine, crude drugs, and health foods (except western medicine) accounts for 16.7%∼84.2% of drug-induced liver injuries, diffe-rences exist between those studies, and many problems exist in the methodology [7]. In most cases, it is difficult to determine whether the selection criteria for drug-induced liver injury is exactly applied as a retrospective study, and in addition to inaccuracies in the definitions of herbal medicine, crude drugs, and plant medicine, the studies focused on frequency comparis-ons of western medicine vs materials other than western medi-cine. In addition, a large number of studies failed to identify the types of western medicines in detail [7].
The data on the causes of liver injury could be misunderstood because of the researchers’ prejudice because they looked for the causes of liver injury at this current time when the liver inju-ry must have occurred in the past. For such a reason, there is a big difference in the results between researchers who studied liver injury [18]. In particular, when an investigation is conducted by researchers who have a negative perspective on herbal med-icine, an unclear abnormal liver function is likely to associated with herbal medicine. According to clinical research on 237 participants conducted in 2006, 10.1% of the patients who were hospitalized at a traditional herbal medicine clinic for a treatment of herbal medicine showed an abnormal biochemical liver function in a test when it was initially tested. Given the low prediction of 'positive' liver function on a liver disorder test which is clinically significant [19], about 10% of the subjects can be taken as being abnormal patients whose cause of disease used unclear on the biochemical liver function test. Also, accor-ding to a thesis, 7.8% show an abnormal liver function. This indi-cates that the risk of liver injury caused by herbal medicine can be exaggerated if abnormal liver function subjects who showed no symptoms although they existed are not considered [20].
This study was conducted on patients who were hospitalized with the diagnosis of nervous system disorders and other major symptoms from January 2011 to August 2011 and had no conge-nital liver function disorders. A retrospective analysis was cond-ucted on the basis of charts of patients who had no abnormal case in other areas on their blood tests during their hospitaliz-ation and who showed an abnormal result only on their liver function tests. Those patients were classified into three groups: a group of patients who took herbal medicine properly at a traditional herbal medicine clinic after the liver function test; a group of patients who took medicines in combination of herbal medicine, medication for liver disorder, and liver protective age-nt; a group of patients who took medicines in combination of medication for major symptoms, medication for liver disorder, and liver protective agent at a western medicine ward. Then, 30 individuals were randomly selected from each group. Thereafter, AST, ALT, ALP, and T-bil before and after taking the medicine were compared for analysis.
The mean age of the entire 90 participants was 57.67±13.75 years old. There were 45 males and 45 females. The duration of medicine administration was 14.67±10.68 days. The cerebrov-ascular disease showed the highest proportion at 67%, and facial paralysis accounted for 14%.
In the herbal medicine group, AST was reduced significantly from 49.77±24.86 to 29.80±11.05 and ALT from 56.10±17.53 to 34.50±19.56 (p < 0.01). ALP was increased slightly from 69.20±19.54 to 74.80±34.08 and T-bil was reduced slightly from 0.81±0.55 to 0.76±0.30, but their differences were not significant (Table 2). In the western medicine group, AST was reduced significantly from 65.77±27.43 to 30.80±9.79 and ALT from 75.47±36.87 to 28.60±14.59 (p < 0.01). ALP was reduced sligh-tly from 88.54±34.17 to 79.93±19.72 and T-bil from 0.76±0.72 to 0.66±0.28, but their differences were not significant (Table 3). In the herbal/western combined medicine group, AST was reduced significantly from 60.73±35.94 to 37.87±15.46, ALT from 89.37±12.97 to 34.20±12.97 and ALP from 76.97±24.26 to 65.70±20.15 (p < 0.01). T-bil was reduced slightly from 0.75±0.25 to 0.67±0.20, but without significance (Table 4). This indicates that all three groups showed a reduced ALT via a proper treatment, that the recovery of liver function can be expected, and that all three groups showed a significant result in the reduction of AST and ALT.
As to difference before and after taking medicine, AST was reduced level by 19.97±22.81 in the herbal medicine group, by 34.97±30.79 in the western medicine group, and by 22.87±33.84 in the herbal/western combined medicine group. The western medicine group showed a more significant reduction (p < 0.05) than the herbal medicine group, the herbal/western combined medicine group showed more reduction than the herbal medicine group, and the western medicine group showed more reduction than the herbal/western combined medicine group, but their differences were not significant. ALT was reduced level by 21.60±23.53 in the herbal medicine group, by 46.87±37.33 in western medicine group, and by 55.17±36.97 in herbal/western combined medicine group, and the western medicine group and herbal/western combined medicine group showed a more significant reduction (p < 0.01) than the herbal medicine group. The herbal/western combined medicine group showed more reduction than the western medicine group, but the difference was not significant. ALP was reduced level by -5.60±21.49 in the herbal medicine group, by 8.60±27.71 in the western medicine group, and by 11.27± 12.63 in the herbal/western combined medicine group. The western medi-cine group (p < 0.05) and the herbal/western combined medicine group (p < 0.01) showed each more significant reduction than the herbal medicine group and the herbal/western combined medicine group showed more reduction than the western medicine group, but their differences were not significant. T-bil was reduced level by 0.05±0.41 in the herbal medicine group, by 0.10±0.50 in the western medicine group, and by 0.08±0.18 in the herbal/western combined medicine group, but there no significant difference existed between the three groups.
Given the changes in AST and ALT, the western medicine group and the herbal/western combined medicine group showed a significant reduction in the values than the herbal medicine group. In general, the western medications seem to be effective as they only focus on the ALT itself. In addition, ALP was reduc-ed significantly in the western medicine group and the herbal/western combined medicine group compared to the herbal medicine group. In most cases, the reduction was within the range of normal values, so it can be seen to be a meaningful comparison. On the other hand, as the herbal/western combin-ed medicine group showed an improvement in the recovery of ALT similar to the western medicine group, the currently eme-rging herbal/western combined treatment seems to be showing a positive prospect.
During the hospital treatment for major symptoms, all three groups showed abnormal liver function on blood tests. Western medicine, herbal medicine, and combined medicine were all effective for minor liver function disorders, no side effects on liver injury were noted for single administration of herbal med-icine, and treatment for major symptoms without worry about liver injury was possible even with an addition of herb medicines. Furthermore, it was found that continuous herbal medicine administration by a proper modification was found to be helpful in the recovery of liver function.
This study showed that although a patient shows an abnormal liver function during administration of herbal medicine, he/she can be treated by a proper addition of a single drug without stopping the administration and that continuous treatment of major symptoms is possible without increasing ALT by were combined administration of a medication for liver disorder and a liver protective agent. Rather than side effects, this study showed an effect of recovery when ALT were increased, but as it was a retrospective study, limitations exits. The period of administration was not equal, patients did not have a single disease, and the types of medicinal herbs were not controlled. Thus, further prospective studies on the liver function test are necessary, with control groups both for herbal medicine and western medicine.
A retrospective study was conducted in patients who were hospitalized at Dong-Eui Hospital from January 2011 to August 2011 and had an abnormal liver function on a biochemical seru-m test. They were randomly selected and classified into a herbal medicine group, a western medicine group, and a herbal/we-stern combined medicine group. Our findings are as follows:
1. Both in the herbal medicine group and the western medicine group, AST and ALT after treatment were reduced signifi-cantly compared to AST and ALT before administration, and in the herbal/western combined medicine group, AST, ALT, and ALP after administration were reduced significantly compared to AST, ALT, and ALP before administration.
2. In LFT changes before and after administration, AST (p < 0.05), ALT (p < 0.01), and ALP (p < 0.05) reduced significantly in the western medicine group compared to the herbal med-icine group, and ALT (p < 0.01) and ALP (p < 0.01) were redu-ced significantly in the herbal/western combined medicine group compared to the herbal medicine group. There was no significant difference between the herbal/western combined medicine group and the western medicine group.
3. In LFT changes before and after administration, AST and T-bil showed no significant difference between the herbal medicine group, the western medicine group, and the herbal/western combined medicine group, but ALT (p < 0.01) and ALP (p < 0.01) were reduced significantly in the western me-dicine group and the herbal/western combined medicine group compared to the herbal medicine group.
Taken together, both herbal medicine and western medicine were effective for the treatment of liver function disorder. In ge-neral, for the western medicine group and the herbal/western combined medicine group treatment was more effective than for the herbal medicine group, but the difference between the western medicine group and the herbal/western combined medicine group was not significant. In addition, no liver injury was caused by the administration of herbal medicine; rather, the use of herbal medicine for treating major symptoms was helpful for the recovery of liver function.