The spontaneous regression of herniated cervical discs is not a well-established phenomenon. However, we encountered a case of a spontaneous regression of a severe radiculopathic herniated cervical disc that was treated with acupuncture, pharmacopuncture, and herb medicine. The symptoms were improved within 12 months of treatment. Magnetic resonance imaging (MRI) conducted at that time revealed marked regression of the herniated disc. This case provides an additional example of spontaneous regression of a herniated cervical disc documented by MRI following non-surgical treatment.
Since Guinto, et al. reported a case of spontaneous regression of a herniated lumbar disc in 1984 [1], this phenomenon in lumbar discs has been well documented and discussed [2-4]. However, there have been fewer reports of spontaneous regression of cervical disc herniation (CDH) [5-7], especially ones confirmed by magnetic resonance imaging (MRI) [8-10]. Recently, a patient with CDH who was treated at our hospital experienced this exceptional condition after 12 months of conservative treatment. In the following report, we will present this case and discuss the condition.
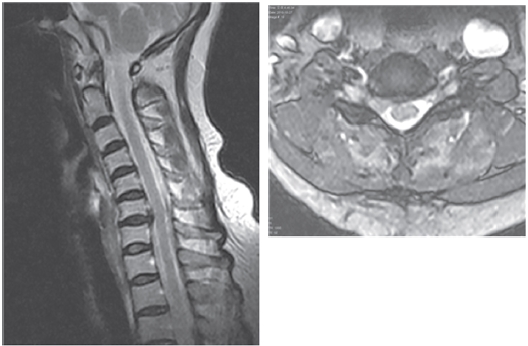
A 59-year-old female patient who was unable to conduct her normal activities or sleep due to intense neck pain and severe radiating pain in the right C7 dermatomal distribution was admitted to our institute a day after her symptoms developed. The patient had a preference for traditional Korean medicine. Despite analgesic injection, she could not maintain a supine position owing to insufferable pain from the day of admission. MRI at 15 days after the admission (Fig. 1) revealed multiple degenerative changes of the cervical vertebra, as well as a disc that was significantly herniated to the right at the C6-C7 level. On physical examination, her motor power (esp. wrist flexion) was assessed as grade 4+; the Spurling test was positive on the right side.
Details of the treatment are reported in Table 1 based on the Standards for Reporting Interventions in Clinical Trials of
Acupuncture(STRICTA) [11]. She received individualized acupuncture treatment that focused on specific symptoms. The most frequently targeted local points were GV16, BL11, TE10, GB20, BL10, and GB21, BL12 and the most frequently treated distant points were SI3, TE3, and LI4. She could barely sleep for the first two weeks. She received analgesics, non-steroidal antiinflammatory drugs and a muscle relaxant for only four weeks. She also received physiotherapy over a period of 5 weeks while admitted.
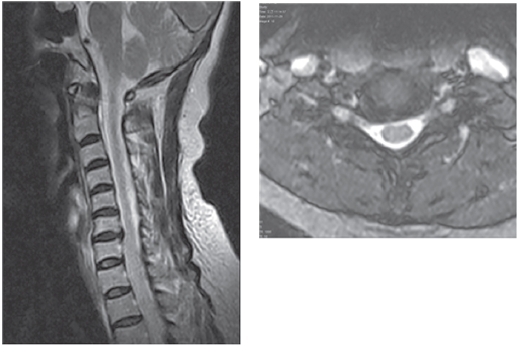
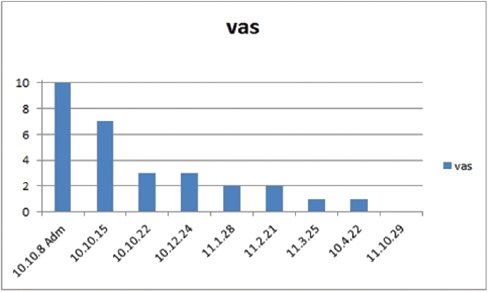
The patient's visual analog scale (VAS) score improved from 10 points at the time of admission to 3 points after 2 weeks of treatment (Fig. 3). After 12 months, the patient's symptoms were completely alleviated, and no abnormal sensory, motor or Spurling test findings were observed. In addition, follow-up MRI conducted after 12 months revealed that the protruded disc had disappeared completely and that no root compression was present (Fig. 2).
Since the first report of spontaneous regression of a herniated cervical disc by Krieger and Maniker in 1992 [5], several other authors have also reported this rare phenomenon [6-10]. According to the guidelines of the U.S. Department of Health & Human Services [13], anterior surgical nerve root decompression via anterior cervical discectomy with or without fusion in patients with cervical radiculopathy is recommended for rapid relief (within 3-4 months) of arm and neck pain, weakness, and/or sensory loss compared to physical therapy or immobilization with a cervical collar. In the absence of knowledge about the natural history of a herniated disc, doctors are apt to choose surgical treatment. However, surgical intervention of the cervical spine can cause serious complications. Fountas et al. [14] published a retrospective review of complications associated with an anterior cervical discectomy and fusion in 1,015 patients. The results of their studies revealed a mortality rate of 0.1% and a morbidity rate of 19.3%, with the most common complication being development of isolated postoperative dysphasia, which was observed in 9.5% of the patients. Other complications observed included postoperative hematoma (5.6%), recurrent laryngeal nerve palsy (3.1%), dural penetration (0.5%) and esophageal perforation (0.3%).
The possibility of such complications makes non-surgical treatment for cervical disc herniation desirable. Spontaneous regression of CDH with acupuncture treatment can be regarded as a benign natural course that occurs in some patients with herniated cervical disc. Several traditional Korean medical methods have been used to treat herniated cervical discs. Lee et al. [15] reported that Carthmi-Flos herbal acupuncture therapy improve the symptoms. He evaluated 20 cervical disc herniation patients treated using Carthmi-Flos herbal acupuncture. The result of his study revealed 30% excellent, 35% good, and 35% fair. Kim et al. [16] used MRI to confirm that spontaneous regression of a herniated cervical disc had occurred in 9 patients after traditional Korean medical treatment, including acupuncture, bee venom pharmacopuncture, manipulation, and herb medicine. Shin et al. [17] reported clinical improvement made by bee venom therapy at cervical hyeopcheokhyeol in the case of upper limb disability caused by cervical herniations.
Many factors related to the regression process have been recognized, including the age of the patient, dehydration of the expanded nucleus pulposus, resorption of a hematoma, revascularization, penetration of herniated cervical disc fragments through the posterior longitudinal ligament (PLL), the size of disc herniation, and the existence of cartilage and annulus fibrosus tissue in the herniated material. Resorption of a herniated nucleus pulposus is thought to occur via an inflammatory reaction in the outermost layer of the herniation, with macrophages as the major cellular population [18].
Acupuncture could be a useful method to facilitate the factors we mentioned. Although we report only one case of CDH, it might give clinical doctors a chance to reconsider surgery, and choose conservative treatment.
Here, we report a case in which a cervical disc herniation patient improved in response to acupuncture. MRI conducted to evaluate the patient 12 months after treatment revealed that spontaneous regression of the herniated disc had occurred. Acupuncture may be considered as an option for the treatment of patients with CDH.