Conditions like anaemia, vitamin A and iodine deficiency continue to pose a major health challenge for growing children and adolescents especially in developing countries like India, even after scientific advances in treatment strategies. In spite of its technical feasibility, the transient methodology of providing supplements with food has not been effective in developing world due to issues with delivery and compliance (Ahluwalia, 2002).
A range of distinctive factors from nutritional deficiencies of iron, Vitamin A, B12 and folate to malaria and chronic inflammatory disorders can cause anaemia (Clark, 2008). However, the most severe consequence of iron depletion is Iron Deficiency Anaemia (IDA).
IDA is a commonly occurring nutritional deficiency worldwide generally arising when body’s iron demands are not met due to inadequate intake, impaired absorption or transport, physiologic losses associated with reproductive age, or post disease chronic blood loss (De Maeyer et al., 1989).
Iron deficiency is very common amongst infants and young children that have profound adverse effects on their development patterns (Vijayaraghavan et al., 1990). Nutritional intake during childhood has a huge impact on a child’s present and future health (Kanani et al., 1997). High iron requirement of the body, if not met, makes early childhood one of the highest risk period for iron deficiency (Domellof et al., 2014). Along with causing symptoms such as tachycardia, dizziness, shortness of breath and fatigue, anaemia also leads to cognitive delays and poor achievement scores (Kotecha et al., 2002).
Iron deficiency is a global health issue and prevention or treatment, particularly in children in developing countries, is a major health challenge. Nutritional anaemia adversely affects the mental and physical health of children and also, causes an increase in morbidity. Furthermore, providing iron supplements in later ages may not be effective in combating the effects (Kapil, 2003). A national nutritional anaemia control program was launched to test the effects of iron supplementation in pregnant women, in India, when given after first trimester of pregnancy. The supplementation, however, failed to bring any significant increase in their body’s iron content, suggesting that it is important to maintain iron store of a women before she is pregnant (Deshmukh et al., 2008). Despite all efforts made in this regard, nutritional anaemia continues to be a severely major health issue, suggesting that the efforts have been ineffective.
High prevalence of anaemia has been reported among Indian adolescent girls (Shobha and Sharada, 2003). However, adolescent school children are a neglected group in terms of micronutrients interventions strategies aimed at preschool children or pregnant women (Pollitt et al., 1985). There is not much change as in 2010, the overall prevalence of anaemia was noted to be 32.9% with an increase in incidences in children below the age of 5 years, over a period of 10 years (Kassebaum et al., 2014).
An earlier study with non iron containing Ayurvedic preparations
This study was conducted from February to November 2006.
Single blinded, randomized controlled clinical trial: Ethical clearance and permission: the principal and teachers of all the schools involved were given a detailed briefing on the study protocol. Prior permission was taken from the management of all the three schools for conducting this study. This study was approved by State Government of Uttarakhand and a state level committee comprising of experts from Department of Health, Department of AYUSH, Ministry of Health and Department of Education and Administration was formed to approve the study protocol and periodic monitoring of the progress. Free and informed verbal consent of the students and their parents was taken before the start of study.
Haemoglobin estimation was done by cyan meth-haemoglobin method. Internal quality assurance program was carried out periodically for consistency. External quality assurance program was carried out by exchanging samples with laboratory of Department of Human Nutrition and Gastroenterology, All India Institute of Medical Sciences, New Delhi. Anaemia was diagnosed as per WHO recommendation.
A total of 1014 school students comprising of 598 girls and 416 boys (11 - 18 years) were initially screened for the study from 8 different schools:
Total number of anaemic students (n = 820) were then divided randomly into four groups with a specific treatment each. The students were blinded to the treatment assignment.
The Ayurvedic medicines
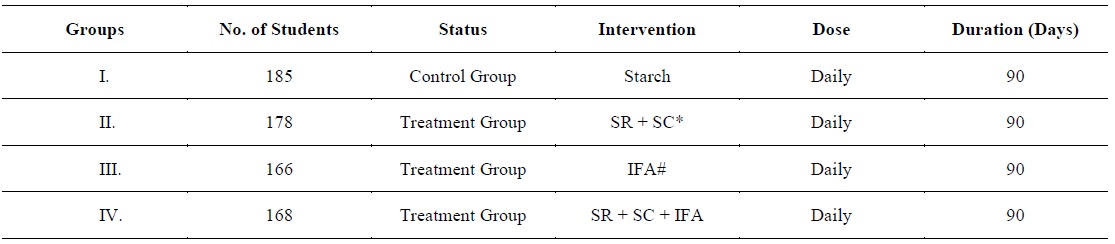
The study comprised of 820 students. Participating students of group I were given starch and acted as control group. Group II participants received Ayurvedic preparations (SR 250 mg + SC 400 mg), group III received 100 mg elementary iron and 500µg IFA, group IV students received (SR 250 mg + SC 400 mg) along with IFA. On the first day (day 0), blood samples were drawn from all subjects for haemoglobin (Hb) estimation. Thereafter, Hb estimation was done on day 30, 60, 90, 170, and 270 respectively. All the drugs were orally administered as per the schedule given in Table 1.
[Table 1.] Various study group and treatment schedule
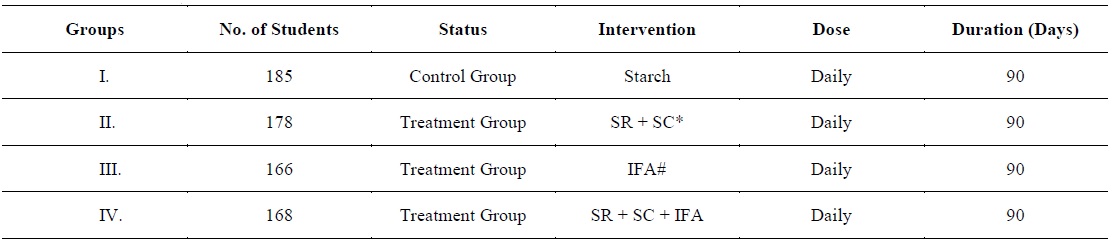
Various study group and treatment schedule
The enrolled students were followed at weekly interval for the treatment period. The field staff visited all the schools regularly to supervise the consumption of the medicines to ensure maximum compliance.
The data was analysed by SPSS software (version 12.0, SPSS, Chicago, IL, USA). Mean and 95 percent confidence interval in each group were calculated. A paired test was used to calculate the change in Hb levels within the group. One way ANOVA was used for multiple comparisons among the groups.
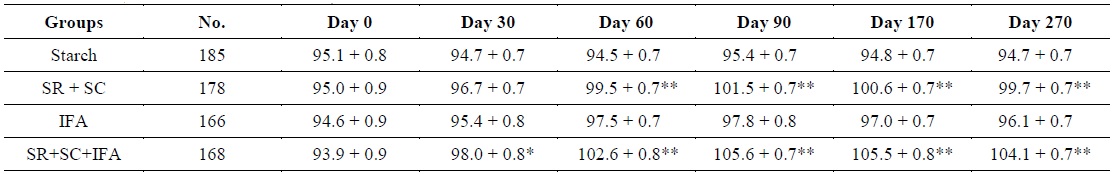
Around 80.8% of the total students studied (i.e. 820 out of 1014 students) were found to be anaemic. A total of 78.6% (327) were boys while 82.4% (493) were girls. The haemoglobin concentration of the various intervention groups at different time periods are given in Table 2. At baseline, the mean haemoglobin concentration of various groups was 94.7 ± 12.2 g/L and ranged from 93.9 ± 0.8 g/L to 95.1 ± 0.8. After 30 days of treatment, significant increase in Hb concentration was observed in group IV. At the end of treatment period, significant differences were noted within and amongst all the treatment groups. Group II (SR 250 mg + SC 400 mg) and group IV (SR + SC + IFA) were found to be better than the group III (IFA). However, the increase in Hb levels in group IV was significantly higher than any other group. At the end of study period (270 days), the mean gain of Hb level (g/L) in the three intervention groups II, III, and IV were 4.6 ± 0.4, 1.4 ± 0.3, and 10.1 ± 0.6 g/L, respectively. The maximum gain was noted in the group IV which was significantly higher than any other group. At the end of study period, 123 students dropped out due to various reasons viz. non compliance, parental objection or lost to follow-up. However, no adverse effect of the Ayurvedic medication was recorded in any of the participants.
[Table 2.] Haemoglobin Concentration in g/l (Mean ± SE) of all groups from baseline to end of study
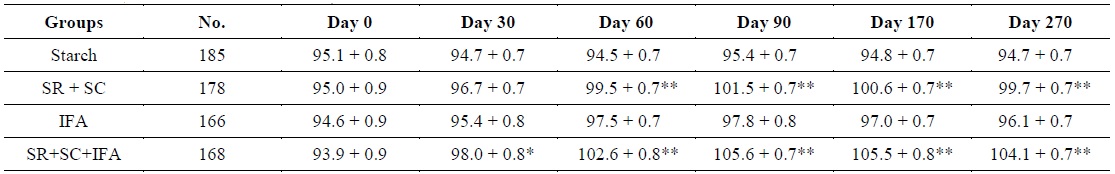
Haemoglobin Concentration in g/l (Mean ± SE) of all groups from baseline to end of study
Deficiency of essential micronutrients like vitamin A and iron is very common in Asia. Iron deficiency anaemia affects 40 - 50% of preschool and primary school children (Khor, 2003). A very high prevalence of IDA has also been estimated in adolescents. Literature survey of Srihari et al. indicates that occurrence of anaemia ranges from 19 to 88% across five different cities in India (Srihari et al., 2007). According to a national survey, 79.2% children under 3 years of age and 56.2% of women (aged 15 - 49) have anaemia (Toteja et al., 2006). High prevalence of anaemia (around 80.6%) was seen in adolescent students (Ramachandran P, 1989).
The present study indicated that non iron containing Ayurvedic formulations
A study hypothesis seldom explains the cause of anaemia. In general, iron deficiency results when iron demands of body are not met due to insufficient intake, poor absorption, impaired transport, physiologic losses or chronic blood loss as a result of disease (De Maeyer et al., 1989). Therefore, diet plays an important role in restoring iron deficiency. However, Indian diet predominantly comprises of cereals which are grossly deficient in protective foods. Serious nutritional inadequacies results in low birth weight, retarded growth, and nutritional deficiency (Viteri, 1998). When diet alone cannot restore deficient iron levels to normal within an accepted frame, iron supplementation has to be provided (De Maeyer et al., 1989). Supplemental iron is available in two forms: ferrous and ferric. Ferrous iron salts are the best absorbed form of iron supplements. Many studies have suggested that a supplement administered twice in a week or even once is as effective as daily supplementation in raising Hb levels (Yip et al., 1988; Yusufji et al., 1973).
In the past, many daily supplementation programs in developing countries have been unsuccessful due to lack of supply and compliance (Galloway and McGuire, 1996). Despite the efficacy and low cost of the ferrous preparations, they are associated with side effects such as nausea, epigastric discomfort, and constipation (De Maeyer et al., 1989). However, in the present study no notable adverse side effects of Ayurvedic for ions were noted in any treatment group.
Iron is a component of every living cell and is essential in the maintenance of health (De Maeyer et al., 1989). It plays a central role in oxygen transport and cellular energy metabolism. The significance of ensuring adequate bio available dietary iron stems from the severe consequences associated with iron deficiency and anaemia, including reduced immune function and resistance to infection, formative delays and irreversible psychological deficiencies in young children, impeded physical work performance, and adverse pregnancy outcomes (Cooper et al., 2006). The quantity of bio available iron is important in diet. This is determined by simulation and inhibitory factors that exist within a meal (Bothwell et al., 1989). Iron supplement should be taken with a source of ascorbic acid such as orange juice as acidic environment facilitates better iron absorption, whereas, food products containing tannins and phytates, such as tea, that reduce iron absorption should be avoided. Also, medicines, such as antacids, proton pump inhibitors, h-blockers, that raise the gastric pH need to be avoided (De Maeyer et al., 1989).
The rationale of using non iron Ayurvedic preparations SS and IFA together was that SS may improve the absorption of iron in gastrointestinal tract. The result from this present study indicates maximum gain of Hb was seen among the participants given SR+SC+IFA. Our present experience and earlier studies indicate that combination of
Adolescence represents a real opportunity to make a difference in life-long patterns (Kaur, 2006). Though there is lot of interest globally in adolescent reproductive health and sexually transmitted diseases, adolescent nutrition has also aroused little interest (Kurz, 1996). Adolescent girls living in developing countries like India constitute a vulnerable group; they get married at an early age and are exposed to greater risk of reproductive morbidity and mortality. However, little attention is given towards the nutritional deficiency in adolescent students. A reason for this inadequate attention may be reluctance to target a new group when even interventions for the primary target group, i.e., pregnant women through prenatal care services, are not functioning adequately. Despite the fact that this pragmatic concern ought not to be taken lightly, it is primarily a logistical supply issue deserving reliable consideration, regardless of additional target group (Kurz and Galloway, 2000). Evidence suggests that control of anaemia in pregnant women may be more easily achieved if satisfactory iron status can be ensured during adolescence (WHO, 1999). To conclude, different causative factors lead to higher incidences of anaemia in developing countries (Tolentino and Friedman, 2007). Nutritional disorders are responsible for most of mortality and drop outs among adolescent students in India (Awate et al., 1997). Evidence suggests that preventive supplements coupled with nutrition education may be a more effective strategy associated with better compliance and improvement of iron status (Ahluwalia, 2002). Our study indicates that there is high prevalence of anaemia in both school going boys and girls. Adolescent health is the most important indicator of development of a nation. Hence, urgent attention is required in this area as proper interventions in school students have shown to improve anaemia.
The result from our study indicates that non iron Ayurvedic preparation
The authors have no conflicting financial interests.