Osteoporosis is known as a “silent thief” whose symptoms do not manifest until fractures occur unexpectedly, often from minimal trauma(Kalu, 1991; Lauritzen, 1996; Melton and Cummings, 1987). When osteoporotic conditions persist, the risk of fractures in the femoral neck, spine, or distal radius, among other areas, increases(Kalu, 1991; Lauritzen, 1996; Melton and Cummings, 1987). Although osteoporosis is on the rise as a societal problem in Western countries, the lower diagnosis and treatment rates in Asia seem to reflect a lack of awareness about its severity among Asians(Choi
In normal adults, bone goes through a process of continuous remodeling, consisting of periods of formation and destruction. Bone remodeling is mediated by osteoclasts, which are cells that resorb bone, and osteoblasts, which are cells that form bone. In bone remodeling, if osteoclastic activity predominates, bone formation decreases and bone remodeling cannot be maintained. As a result, underdeveloped bone cells become prevalent, bones become porous and fragile, and osteoporosis develops.
Risk factors for osteoporosis include female sex, advanced age, low calcium and vitamin D intake, genetic factors, smoking, alcohol abuse, low BMD, low body weight, recurrent falls, personal history of fracture, race or ethnic background, and insufficient physical activity. Despite the wide range of risk factors, the fact that postmenopausal, middle-aged women make up most of osteoporotic population suggests that estrogen deficiency may be the leading cause of osteoporosis(Lim
One of the most commonly used methods for antiresorptive therapy is alendronate, a bisphosphonate class drug that effectively treats osteoporosis by inhibiting osteoclastic activity (Imai, 2013). Alendronate inhibits farnesyl diphosphate synthase (FDPS), an enzyme necessary for the formation of the cytoskeleton in osteoclasts. When FDPS is inhibited, protein geranyl-geranylation is suppressed (Imai, 2013; Goffinet
The author reported that silk fibroin hydrolysates might be a new candidate for the prevention and treatment of osteoporosis in patients (Kweon
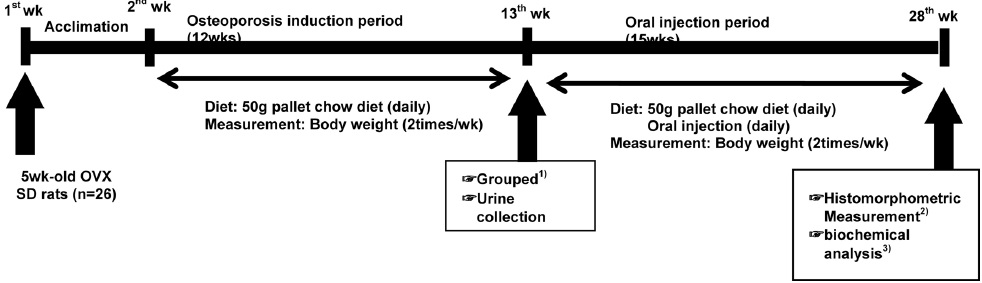
The experimental protocol was approved by The Animal Care and Use Review Committee (IACUC) of Kyung Hee University. (KHUASP (SU) 13-01). Twenty-six Sprague-Dawley rats, all five weeks old, were purchased from SLC, Inc. (Shizuoka, Japan). Twenty-two rats underwent ovariectomy (ligated and excised the ovaries), during which isoflurane inhalation (3% dissolved in oxygen) was used as anesthesia. The remaining four rats underwent sham operations, the purpose of which was to inflict similar levels of stress to the control rats as the ovariectomized ones. Rats were cage-paired in temperature-controlled rooms (22±2℃) with a relative humidity of 55±5% and a 12-h light/dark cycle.
The experimental period lasted 28 wk (Fig. 1). During the first week, a pellet chow diet and tap water were provided
Starting the 14th week of the experimental period, 50 g of pellet chow diet was administered to all groups, and we applied an experimental oral injection to each group until the 28th week. SHAM and OVX groups were orally injected with 2 mL of distilled water. The ALEN group was orally injected with 10mg of alendronate sodium per kilogram of rat once a day. The CT100 group was orally injected with 100 mg of CT per kilogram of rat once a day, and the CT300 group was orally injected with 300 mg of CT per kilogram of rat once a day.
Following the initial week of acclimation, body weights of the rats were measured twice a week. The unconsumed pellet chow was collected and measured at the end of each day. After the end of the experiment period, following 12 h of overnight fasting, the rats were administered intraperitoneal anesthesia with zoletil (0.1 cc/100 g) and rumpun (0.03 cc/100 g), inhalational anesthesia with ethyl ether, and were then sacrificed.
Blood samples were collected using cardiac puncture for serum collection. Serum was isolated by centrifugation (PK121R, Milan, Italy) at 3000 rpm for 15 min at 4℃ and stored immediately at -70℃ until analyzed. Serum calcium (Ca) was measured using a chemistry auto-analyzer (ADVIA 1650, Bayer, Tokyo, Japan), and serum osteocalcin was measured using the MILLOPLEX bone hormone panel (Millipore, Billerica, MA, USA).
Urine was collected on the 14th week (basal) and the 28th week (final) of the experimental period for comparison. Before the collection, the metabolic cages were cleaned with 0.1N of hydrogen chloride (HCL). During the 24-h urine collection period, we limited the rats’ water source to distilled water in order to prevent any contamination of the urine. Collected urine samples were centrifuged at 2,000 rpm for 15 min at room temperature, and the top layer was collected and stored at -70℃ until future analysis.
The urinary calcium and inorganic phosphorus levels were measured with a chemistry auto-analyzer (ADVIA 1650, Bayer). N-terminal telopeptide (NTx) was measured by ELISA using commercial kits (Osteomark, Wampole Laboratories, Princeton, NJ, USA).
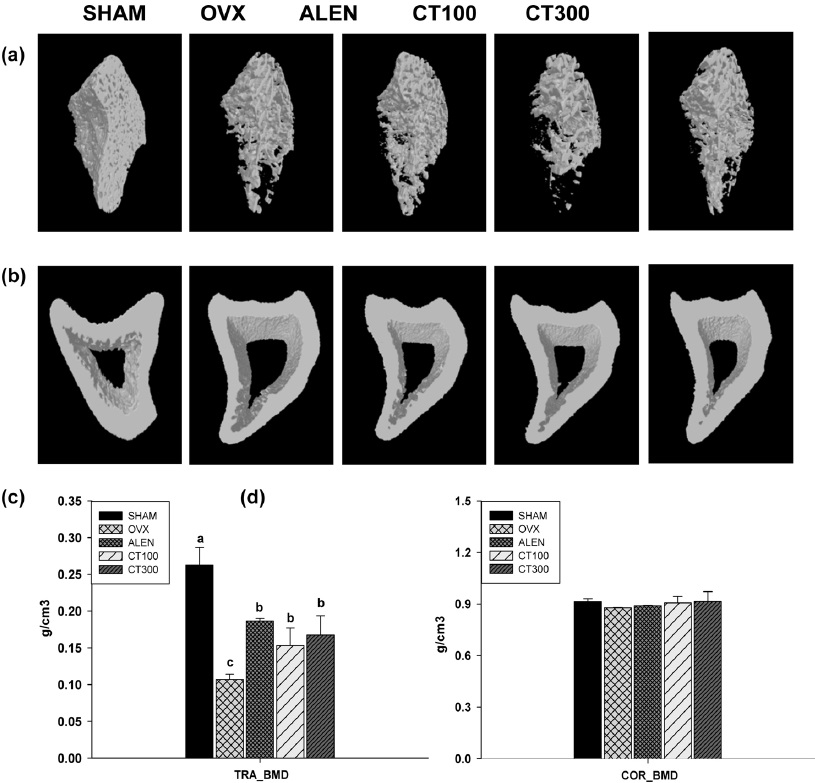
Bone histomorphometric parameters were determined using a Micro-computed tomographic system (μ-CT or micro-CT). At the end of the experimental period, the left femurs of the rats were scanned using micro-CT. Before the scan, the rats were anesthetized with intraperitoneal injections of zoletil 50 (Zoletil 50, Virbac) and rumpun (Rompun, Bayer). After the images were gathered, the cortical and trabecular microstructure were used for 3D reconstruction at 50 kV, 200 μA, at a rotation step of 0.4°. Analysis of the reconstructed scans was conducted using NRecon cone-beam algorithm software (SkyScan), and for three-dimensional analysis and image printing, the files were transferred to the CTan program (SkyScan). Histomorphometric parameters included trabecular bone volume (TRA_BV), trabecular thicknesses (Tb.Th), trabecular number (Tb.N), trabecular separation (Tb.Sp), structure model index (SMI), and trabecular bone mineral density (TRA_BMD).
The means and standard error of measurements (SEM) of each group were calculated using SPSS software (Version 20.0, SPSS Inc, Chicago, IL, USA). Duncan’s multiple range tests followed by ANOVA were performed using
>
Body weight, dietary intake, and food efficiency ratio (FER)
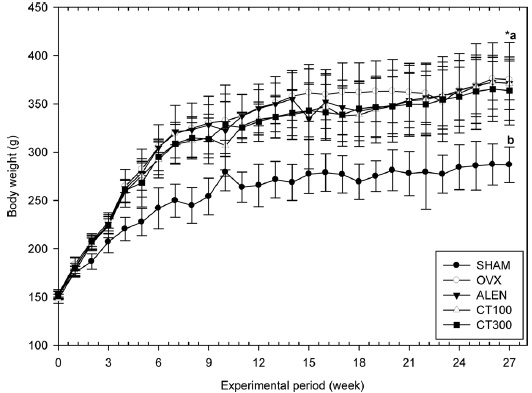
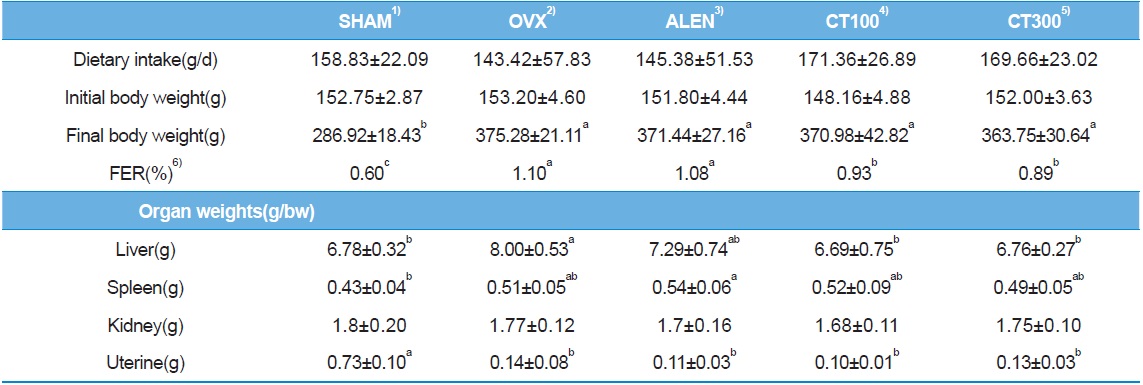
All groups had a similar initial mean body weight (
No significant difference in dietary intake was observed across all groups (
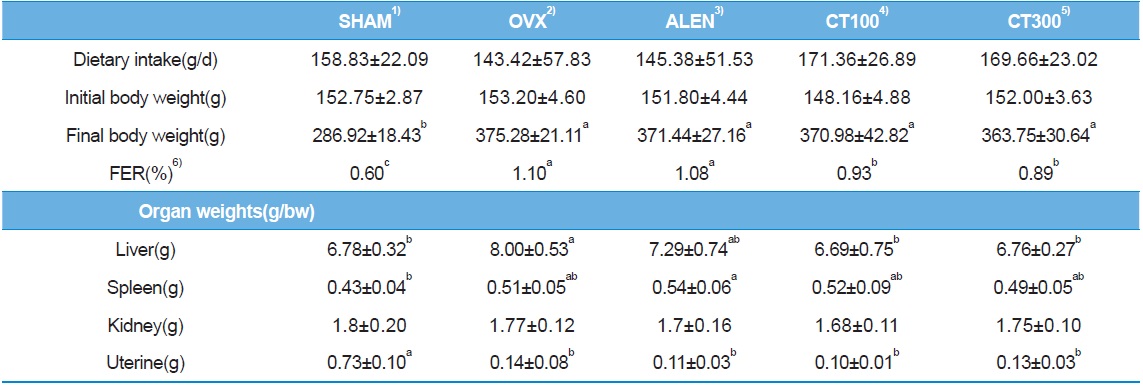
Changes in body weight, weight gain, food efficiency rate, and organ weight in experimental rats
The mean liver weights of the SHAM, CT100, and CT300 groups were significantly lower than that of the OVX group (
>
Biochemical markers of bone turnover
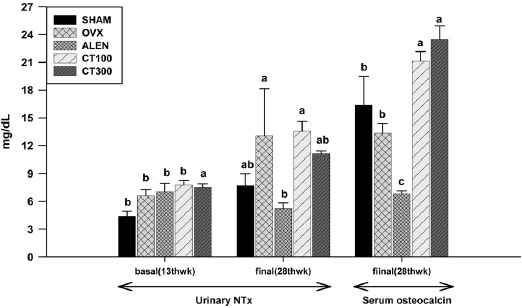
The basal NTx level of the CT100 group was not significantly different than that of the CT300 group, but for the final NTx level measurement, CT intake resulted in a dose-dependent decrease in NTx, with the CT300 group demonstrating a relatively lower NTx level than the CT100 group. The ALEN group showed a reduced level of NTx compared to the SHAM group, and the ALEN group also showed a significantly lower NTx level compared to the OVX group (
The osteocalcin (OC) levels in the CT100 and CT300 groups were significantly higher than that of any other group (
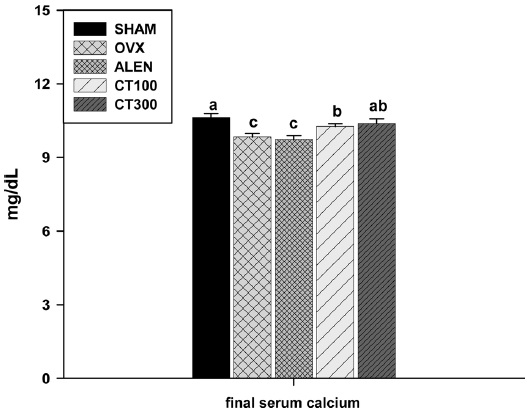
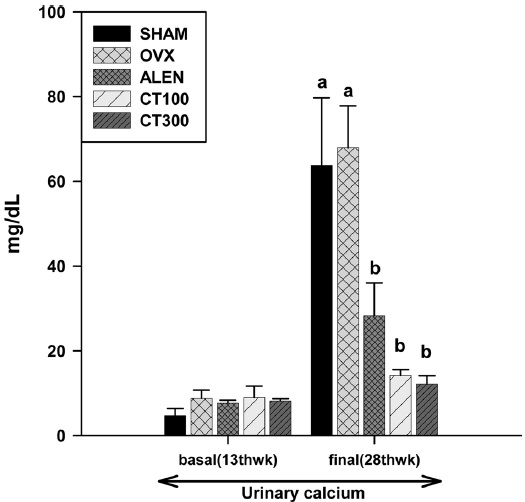
Although showing some significant differences between groups (
According to the basal (14th week) urinary calcium measurements, no experimental groups showed significant differences. However, upon the final (28th week) urinary calcium level measurement, the CT100, CT300, and ALEN groups had significantly lower urinary calcium levels than the SHAM and OVX groups (
>
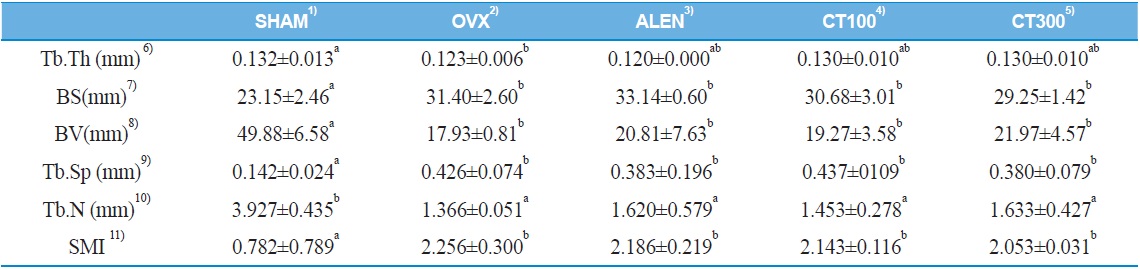
Histomorphometric parameters of trabecular bone
Compared to other groups, the SHAM group showed significant differences in structure model index (SMI), bone surface (BS), bone volume (BV), trabecular number (Tb.N), and trabecular separation (Tb.Sp) (
[Table 2.] Effect of Cudrania tricuspidata on trabecular histomorphometric measurement
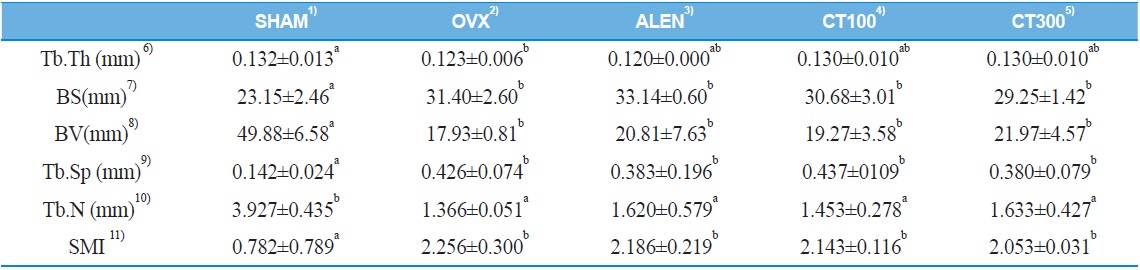
Effect of Cudrania tricuspidata on trabecular histomorphometric measurement
>
BMD of trabecular bone and cortical bone
As seen in Fig.6c, SHAM group manifested significantly higher trabecular bone mineral density (TRA BMD) than the four other groups (
In this study, CT prevented bone loss by inhibiting bone resorption and enhancing bone formation. As a result, CT increased bone health as indicated by biochemical, radiological, and histomorphometric measurements. Therefore, CT extract can be considered as natural treatment for osteoporosis induced by ovariectomy.
As a sensitive biomarker of osteoclastic activity, urinary n-terminal telopeptide (NTx) accurately reflects bone resorption (Ataoğlu
Our data confirmed the effective inhibition of alendronate on osteoclastic activity (Mundy, 1991; Halasy-Nagy
Secreted solely by the bone-building osteoblast cells, osteocalcin (OC) is a convincing marker of osteoblastic activity (Karsenty and Oury, 2013). CT-fed rats showed significantly higher serum osteocalcin (OC) levels, while rats in the ALEN group showed significantly lower OC levels than any other group. This result supports that CT injection stimulates bone formation while alendronate does not affect bone formation because osteoblastic activity reflects bone formation (Karsenty and Oury, 2013). CT’s stimulatory effect on osteoblasts may be explained by the flavonoid in CT, whose effects have been established by previous studies (Li
Although serum calcium levels varied among the experimental groups, they were all within the normal range (Choi and Kim, 2011). Such results do not convey much information about calcium homeostasis, but that calcium homeostasis was functioning properly. However, it is important to analyze what changes in calcium homeostasis ensued, as slight differences between groups could help distinguish the effects of the experimental treatments on bone resorption. To assess these changes in calcium homeostasis, urinary calcium level was examined.
According to our results, urinary calcium was significantly lower among CT-fed rats than in the OVX group, which indicates that CT intake might have improved calcium reabsorption. Because increased renal calcium reabsorption decreases the amount of necessary calcium released from bone to serum, renal calcium reabsorption is an important biological process that is closely related to bone resorption (Nordin, 1997). In other words, increases in calcium reabsorption reduce the need for osteoclastic activity. One way in which CT is suggested to prevent bone loss is via CT’s flavonoid and phosphorus content, which increases calcium and potassium reabsorption and decreases calcium excretion (Chen
Considering the above evidence, we conceived that CT intake could stabilize bone metabolism and improve bone health. For tangible evidence, we analyzed the radiological and histomorphometric measurements of trabecular and cortical bones. While significant differences were not observed in cortical bone measurements across all groups, trabecular BMD, a primary diagnostic indicator of osteoporosis, was higher among the CT-fed groups than in the OVX group, but it was not significantly different between the CT-fed and ALEN groups. Because cortical bone responds slowly to ovariectomy and treatments, these results are reasonable (Mizughuchi
Previous reports suggest that that BMD is positively correlated to serum osteocalcin and negatively correlated to urinary NTx and calcium excretion (Baeksgaaard
The findings in this study are unique in that CT minimizes bone loss by stimulating bone formation and inhibiting bone resorption. Most drugs for osteoporosis are only purported to inhibit bone resorption (Nordin, 1997), but excessive suppression of bone resorption could result in paradoxical effects, such as increases in the fracture risk and reduction of bone strength (Odvina