One of the recent trends in the clinical fields of Korean Medicine (KM) is the application of various meditation techniques centering on Jon Kabat-Zinn’s Mindfulness-Based Stress Reduction (MBSR) to KM psychotherapy1).
Most meditation techniques attach great importance to the process of breathing2); in particular, Breath-counting meditation (Anapanasati, 隨息觀; BCM) is a meditation technique focusing on counting while breathing in and out, i.e., the breath itself is the object of meditation in this technique. BCM has a long tradition in Buddhism, primarily intended to help the meditator concentrate. As the name suggests, BCM involves looking at (觀) what happens in one’s own body and mind while counting(隨) one’s breath (息)3). In most cases, regular and calm abdominal breathing, in which the exhalation time is longer than the inhalation time, is maintained while mentally counting through the duration of the breath (1, 2, 3...)4).
In previous studies related to BCM in KM neuropsychiatry, Chung5) performed a neuro-feedback-based analytic comparison between pre-and post-BCM memory and concentration abilities, and Jung6) and Lee7) investigated the effects of BCM on psychological and physiological states. While there are case studies on representative medication therapy applying MBSR19,20), cases on the clinical application of BCM have not been reported yet.
With this background, the author reports two cases of successful application of BCM for the treatment of patients with anxiety disorder accompanied by panic attacks, and explores the efficacy of BCM in clinical applications.
1. Patients and treatment methods
Two patients with symptoms meeting the Diagnostic and Statistical Manual (DSM-IV) criteria for anxiety disorder with panic disorder underwent BCM-based KM psychiatric treatments and other KM treatments including herbal medicine and acupuncture. The therapeutic effects were evaluated.
The patients were instructed to meditate for 10 min while listening to a record of guided BCM in “Qi-supported 15-minute Meditation”8) by Prof. Kim Jong-Woo of the Department of Neuropsychiatry, Kyung Hee University Korean Medicine Hospital at Gangdong.
The patients were provided with the sound file with the instruction to practice BCM at home every day before falling asleep. They were also instructed to calm down by counting their breaths using the BCM technique whenever they feel the symptoms of panic attacks, such as intense fear and discomfort with palpitations and shortness of breath, breathlessness, and pressure on the chest. Their BCM practice consisted of counting from one to ten and repeating the count at each unit of in-and-out breathing.
Cheon-Wang-Bo-Sim-Dan (天王補心丹; HANPOONG PHARM Co. Ltd.) was prescribed to be taken twice a day, and acupuncture (0.25 mm×30 mm disposable acu needle; Haeng Lim Seo Won) was administered during each clinic visit. Needle retention time was set at 15 min, and acupuncture was performed using a plunger on 中衝 (PC9), 大敦 (LR1), 曲澤 (PC3), 陰谷 (KI10), 內關 (PC6), 少府 (HT8), 太衝 (LR3).
1) PDSS (Panic Disorder Severity Scale)
The author used the Korean version of the Panic Disorder Severity Scale (PDSS). This assessment tool with proven reliability and validity was adapted by Kim et al. in 2001 based on the original PDSS developed by Shear et al. PDSS measures the severity of panic disorder and comorbidity using 7 items. Each item is rated on a 5-point scale ranging from 0 to 4 and the total score is calculated to indicate the degree of panic disorder symptoms.
2) BDI (Beck Depression Inventory)
This self-report questionnaire, which was developed by Aaron T. Beck to assess the presence and severity of depression symptoms, comprises of 21 items pertaining to cognitive, emotional, motivational, and somatic components of depression. Each item is rated on a 4-point scale (0∼3), and a total score is calculated to determine the presence and severity of depression; 0∼9 indicates absence of depression, and 10∼ 15, 16∼23, and 24∼63 points indicate mild, moderate, and serious depression, respectively.
3) BAI (Beck Anxiety Inventory)
This 21-item questionnaire consists of 21 items pertaining to cognitive, emotional, and somatic components of anxiety. Each answer is given a point ranging from 0 to 3, and a total score is calculated to determine the severity of anxiety; 22∼26, 27∼31, and ≥32 points indicate moderate to severe (requiring observation and intervention), very severe, and extremely severe levels of anxiety, respectively.
1) Sex/Age/Occupation
Female/20 years/College student
2) Chief complaints
(1) Extreme fear, shortness of breath, and pressure on the chest from the imagined presence of insects
(2) Constant fear and panic about insects
(3) Insomnia
3) Onset of symptoms
4) Medical history and family medical history
None
5) Current medical history
This 20-year-old female patient had no noticeable medical history and family medical history. The fear of insects began after an insect crept into her ear on September 12, 2013. She cannot enter a room where she sees dust or fruit seeds for fear of insects hiding somewhere in the room. Thinking of or seeing insects results in pressure on the chest and shortness of breath, and she has been to the emergency room three times for extremely severe, life-threatening symptoms. The constant anxiety about being attacked by insects makes her use earplugs to prevent insects from creeping into the ear while she is sleeping. She also suffers from insomnia because of the use of earplugs, which gives her some comfort, but disturbs her sleep, and if she does not use them, she cannot sleep for fear of insects. She also complained of other comorbid symptoms such as lack of appetite, headache, dizziness, and loose stools.
After the diagnosis of phobic anxiety disorder caused by a specific phobia at Hospital S during end-September 2013, she had been medicated (Alprazolam tab 0.5 mg tid). She voluntarily discontinued the medication and visited the emergency room three times with severe symptoms of pressure on the chest and shortness of breath.
6) Social history
She gets easily scared. She tends to follow advice or instruction given by people around her, and has smooth relationships with friends. She has been under stress since the beginning of the summer holidays due to work unjustly imposed by a senior student.
7) Anamnesis
(1) 158 cm/50 kg
(2) Appetite and digestion no appetite and uncomfortable feeling of fullness in stomach
(3) Excretion
- Frequency of defecation and stool form: 1~2 times/day, loose
- Frequency of urination: 7~8 times/day, feeling of incomplete emptying of the bladder
(4) Duration of sleep
- Frequency of urination: 7~8 times/day, feeling of incomplete emptying of the bladder
(5) Tongue diagnosis
red sore tongue with a thin white coating (舌紅苔薄白), teeth marks around the tongue (舌邊齒痕)
(6) Pulse diagnosis
slow and weak floating pulse (脈浮緩無力)
(7) Cold-heat pattern
cold hands and feet, head flushed
(8) Tactile diagnosis
tender points on 膻中 (CV17), 中脘 (CV12), and 關元 (CV4)
8) Catamnesis (clinical course and outcome)
(1) November 22, 2013
After the review and evaluation of personal history, we aimed to establish relationships through empathy and encouragement. The patient scored 22 points on the PDSS, demonstrating severe symptoms of panic attack. The BDI and BAI scores of 19 and 22 points, respectively, indicated high degrees of anxiety disorder and depression.
The patient reported that despite a slight mitigation of symptoms, she discontinued the Alpram tablets for fear of feeling alienated from herself and getting dependent on the medication. I suggested that she should not be afraid of taking Western or traditional medicine. The medication dosage could be adjusted if side effects appeared, and the symptoms would be gradually relieved.
She was taught how to slow down her breathing through BCM whenever overwhelmed by panic attacks during daily activities, and instructed to practice BCM by listening to the recorded sound file every day before sleeping.
(2) November 25, 2013
The patient reported that breath counting alone calmed her breathing, and expressed her surprise and satisfaction. I encouraged her with praise and empathy, and explained that the recurrence of symptoms can be managed by using the same method. She was instructed to rest in a comfortable posture and breathing pattern, and imagine and imprint a safe place in mind. After counseling, she practiced BCM by listening to the recorded guide. She was encouraged to continue the daily meditation before sleeping.
(3) November 29, 2013
The patient reported that the face muscle tension and insomnia disappeared. She thought less about insects and could sleep well despite short disturbances.
Since thinking of insects rendered her less anxious now, she underwent disassociation therapy in which she imagined that an insect approaching the house from the sky was captured and wrapped in a handkerchief, and put in a well-covered corner of the house.
(4) December 2, 2013
The patient reported that the frequency of thinking about insects had reduced and symptoms of shortness of breath and pressure on the chest were considerably less intense. The moment she felt her breathing becoming faster, she applied BCM and counted her breaths, which worked well and made her life much easier.
(5) December 6, 2013
The patient reported that her digestion had improved and she ate more comfortably with fewer incidences of anxiety. She still had occasional anxious moments, but the overall state was stabilized. The next visit was set to take place a month later because of her personal circumstances. I encouraged her to continue the daily meditation before sleeping.
(6) January 6, 2014
The patient reported that she discontinued the medication because her feeling of anxiety had almost disappeared and her daily activities were not affected by it. Seeing insects did not elicit any anxiety, and whenever she felt uneasy, she habitually applied BCM. She also reported that she was practicing BCM every day before sleeping. Her PDSS score fell to 10 points, and BDI and BAI were reduced to 6 and 7 points, respectively.
1) Sex/Age/Occupation
Male/38 years/Buddhist monk
2) Main complaints
Sudden anxieties, shortness of breath, pressure on the chest, and palpitations
3) Onset date
End-February 2014
4) Medical history and family medical history
No noticeable medical history; father with stomach cancer
5) Current medical history
This 38-year-old male patient had his first panic attack at the end of February 2014 while taking a break from physical exercise after a weight reduction dietary meal. He had a sudden feeling of something being terribly wrong and experienced a state of profuse sweating, shortness of breath, pressure on the chest, and weak and unsteady legs. He was overwhelmed by the thought of dying from a heart attack. In Hospital C, he underwent a thorough examination including electrocardiogram and echocardiography, which did not yield any particular findings. During the ensuing 3 weeks, he had three recurrences of the same symptoms while he was taking a meal or a break. He was referred to the Department of Neuropsychiatry of Hospital C, where he was diagnosed with panic disorder with symptoms of panic attack, and received a prescription for medication (Alprazolam tab 5 mg, Fluoxetine 20 mg tid). Three days before he presented to our department, he had the same symptoms of a panic attack with the same feeling that he was about to die. He visited the emergency department of Hospital C, but no particular clinical abnormalities could be confirmed.
6) Social history
Celibate, calm, and clean, he has good relationships with people around him, and has not been recently exposed to any stressful situations.
7) Anamnesis
(1) 169 cm/70 kg
(2) Appetite and digestion
poor appetite, indigestion
(3) Excretion
tendency of constipation
(4) Sleep
sufficient length but of poor quality
(5) Tongue diagnosis
thin white coat on tongue (舌紅苔薄白)
(6) Pulse diagnosis
fine floating wiry pulse (浮緩細)
(7) Cold-heat pattern
head flushed
(8) Tactile diagnosis
tender points on 膻中 (CV17) and 中脘 (CV12)
8) Catamnesis (clinical course and outcome)
(1) March 31, 2014
After the review and evaluation of personal history, we aimed to establish relationships through empathy and encouragement. The patient scored 23 points on the PDSS, indicating highly-severe symptoms. The BDI and BAI scores of 14 and 23 points, respectively, demonstrated an obviously high degree of anxiety disorder and depression.
The patient reported that although the prescribed tablets helped whenever the symptoms appeared and he was in a critical state, he discontinued the medication for fear of not waking up the next morning after the intake of the tablet before sleeping. I encouraged the continuation of medication, assuring him that the side effects were controllable.
He was instructed to do BCM every day before sleeping by listening to the record and to do the BCM breath count whenever he feels palpitations and life-threatening suffocation.
(2) April 4, 2014
The patient reported that he could overcome a sudden panic attack that occurred while showering by applying the BCM. I encouraged him to continue his daily BCM before sleeping, take enough food along with the BCM practice, and reduce excessive physical exercise because the panic attack began after the diet and exercise intervention. I suggested that the diet and exercise intervention he started to improve his health should be replaced by sufficient food intake and rest considering the current body conditions. I instructed him to do BCM with listening to the record.
(3) April 7, 2014
The patient reported that he did not suffer any panic attacks and felt more comfortable than before. He was still worried about heart failure, especially because he was told during the last heart checkup that a coronary artery stricture was suspected although his heart condition was normal. I comforted him by assuring him that a state of perfectly clean coronary arteries is rather rare and the heart never stops by panic attacks, and no sudden death would occur.
(4) April 11, 2014
The patient reported that he could sleep a lot more comfortably and he could calm strange feelings of pre-panic attack in the chest by using the BCM method. He was worried about the possible dependence on the tablets prescribed at Hospital C, which he was taking intermittently. I assured him that there was no reason for worrying about medication because the dose might be gradually reduced to minimize its effect on the body, and BCM could be used for controlling the symptoms.
(5) April 16, 2014
The patient reported that he still felt anxious, albeit significantly lesser than earlier, but indigestion and his appetite had not improved. I pointed out that all such comorbid symptoms would disappear by controlling the panic attack symptoms and that continuing the counteractive behaviors was more important than paying attention to the level of anxiety. I also suggested that he should continue his daily BCM practice before sleeping, and once familiar with it, he should try to expand the breath control to sensitizing the awareness of other body parts and calming the mind.
(6) April 21, 2014
The patient described his current condition as having gradually decreasing anxiety and improved quality of sleep, appetite, and digestion. Since the previous pre-panic attack feelings, no similar symptoms had appeared. PDSS score fell to 12 points, and BDI and BAI scores improved to 6 and 10 points, respectively.
Despite the improvement in the symptom scales, further treatment of residual symptoms and follow-up examination of the clinical course was considered necessary; however, the treatment could not be continued due to the patient’s personal circumstances. I recommended a visit at a later time and continuation of BCM.
A panic attack, a representative symptom of anxiety disorder, can occur in many mental health conditions, such as panic disorder, social phobia, specific phobia, post-traumatic stress disorder, and acute stress disorder. Its key characteristic is experiencing an unexpected extreme fear or discomfort at irregular intervals, with at least 4 of the 13 comorbid somatic or cognitive symptoms such as palpitations, shortness of breath, cold sweats, shivering, breathlessness, suffocation, pressure on the chest, and fear of death. After a sudden onset, the anxiety generally reaches its peak within 10 min. The patients usually try to escape from such conditions and express their overwhelming sense of fear arising from such attempts; for example, they were about to die or believed that they had suffered a heart attack or cerebral hemorrhage12).
In KM, anxiety disorder falls under the categories of fright palpitations (驚悸), fearful throbbing (怔忡), and fear and fright (恐驚), and is interpreted as pattern of deficiency with timidity of heart and gall bladder (心膽虛怯), heart blood deficiency (心血虧損), heart qi deficiency (心氣不足), liver-kidney yin deficiency (肝腎陰虛), phlegm-fluid retention (痰飮內停), and heart blood stasis (血脈瘀阻)13).
The two cases reported above fall under the scope of anxiety disorder involving panic attack symptoms such as palpitations, shortness of breath, breathlessness, suffocation, pressure in the chest, abdominal discomfort, fear of losing self-control, and fear of death. Both patients underwent a BCM-based KM psychiatric treatment supplemented with acupuncture and herbal medicine.
Case 1 was diagnosed with a combined disorder of heart blood deficiency (心血虧損) and phlegm-fluid retention (痰飮內停) caused by heart qi deficiency (心氣不足) based on the symptoms of panic attack caused by insect phobia, generalized fear, insomnia, indigestion, and tender points on 膻中 (CV17), 中脘 (CV12), and 關元 (CV4). Case 2 demonstrated heart blood deficiency (心血虧損) in relation to insufficient food intake and excessive exercise. Therefore, Cheon-Wang-Bo-Sim-Dan (天王補心丹; HANPOONG PHARM Co. Ltd.), which has a therapeutic effect for heart blood deficiency (心血虧損) was administered to both patients.
For acupuncture treatment, given that both cases were confirmed to have a tender point around 膻中 (CV17), which is a 募穴(alarm point) of the 手厥陰心包經 (pericardium meridian: PC), 中衝 (PC9), 大敦 (LR1), 曲澤 (PC3), 陰谷 (KI10) corresponding to the Sim-Po-Jeong-Kyeok (心包正格) treatment, known to mitigate anxiety14) were selected as basic acupoints. 內關 (PC6), 少府 (HT8), and 太衝 (LR3), which are the 原穴 (source point with meridian qi flow) of the 手厥陰心 包經 (pericardium meridian: PC), 火穴 (fire point) of the 手少陰心經 (heart meridian: HT), and 原穴 (source point) of the 足太陰肝經 (spleen meridian: SP), respectively, were selected as supplementary acupoints to strengthen the tonify the heart yin (補心陰).
The therapy for Case 1 focused on the psychological dissociation of the event and the specific phobia-inducing object from “I” to sever the psychological link, aiming at freeing the mind from the fear of insects by inducing a comfortable state of mind in the presence of insects. In Case 2, focus was on dissociating the excessive link between physical symptoms and heart disease by resolutely supporting the anxiety, and not the disease, as the cause of the somatic symptoms.
The underlying principle of psychiatry in KM is I-Jeong-Byeon-Gi therapy (移情變氣療法), which means changing (變) qi (氣) by moving (移) essence (精). It is defined as “achieving the therapeutic goal by changing the patient’s state of mind and repairing the confused state of qi function using the given method”15). It is largely divided into two categories: dissipating the patient’s mental activities in different directions using communicative methods such as language and music (精神轉移法) and inducing the desired emotive state using non-communicative methods such as meditation and self-discipline (情緖導引法). Meditation, belonging to the latter category, aims at achieving and maintaining a healthy body and mind by psychological stability and physical relaxation. It is efficient in reducing anxiety, anger, and stress and thus, used in a wide range of therapies. This is consistent with the holistic viewpoint of the mind-body (心身) medicine representing the KM principle that human physiology and pathology is closely associated with human mental activities. It is also in good agreement with the use of KM psychiatry as a method of stabilizing essence (精), qi (氣), and mind (神) and controlling the mind (調神) through sensitization of seven emotions (七情) of joy, anger, sorrow, fear, love, hate, and desire16,17).
Among many meditation techniques, BCM has breath as the object of complete focus. In BCM applied in KM, the attention is entirely focused on one’s own breath while repeatedly counting the exhalations, while fully sensitized to the sensation of the air passing through the nose, the freshness of the inhaled breath, and the warm temperature of the exhaled breath. A cycle of counting from one to ten is repeated continuously 3). In this process, if the exhalation becomes naturally longer than inhalation, the body is automatically (without any further efforts) relaxed and abdominal breathing takes place. This is conducive to the sensitization of the inner state of body and mind; as a result, the relaxation of the body and self-contemplation takes place simultaneously18).
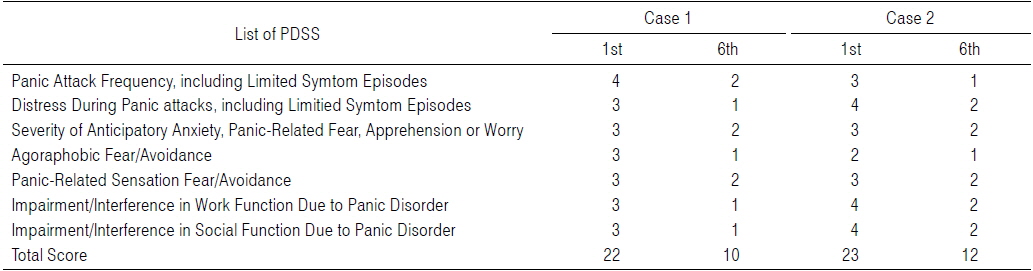
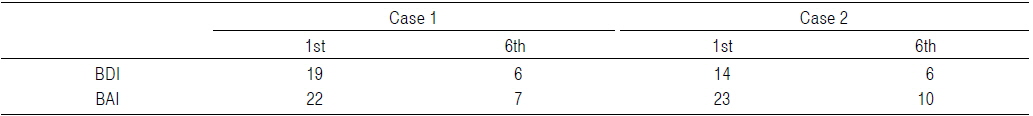
BCM was applied to these two cases by training the patients to practice it during each visit and instructing them to continue it at home every day before sleeping. MBSR, a meditation method most widely applied as a meditation therapy, and BCM applied to the two cases in this report focus on breathing during meditation2) and are known to be efficient in reducing stress7). In both cases, the comparison of pre-and post-intervention PDSS scores (Table 1) demonstrated the improvement of clinical symptoms, and its general stress-reducing effects could be confirmed by the reduced BDI and BAI scores (Table 2).
[Table 1.] Changes of Panic Disorder Severity Scale (PDSS)
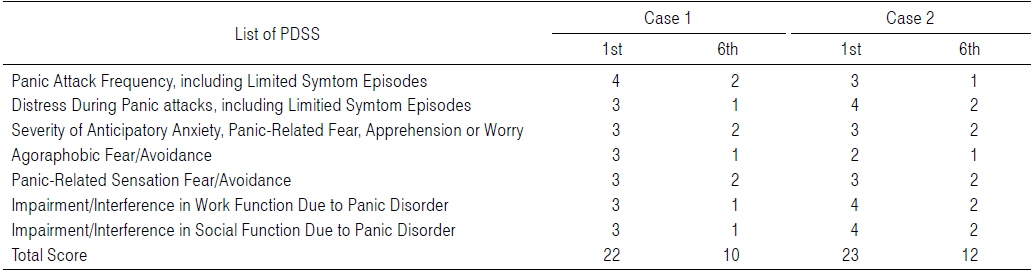
Changes of Panic Disorder Severity Scale (PDSS)
[Table 2.] Changes of Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI) Scores
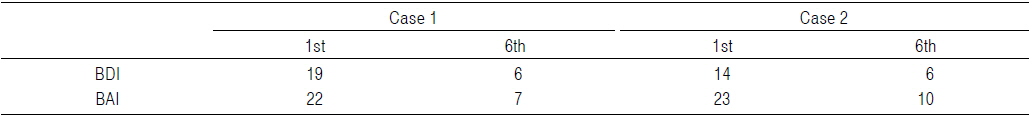
Changes of Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI) Scores
Cases of MBSR application to somatic and psychological symptoms of Hwabyung19) and post-traumatic stress disorder (PTSD)20) have been reported previously, but no case reports have been published to date on panic attack symptoms. This report is different from the currently available MBSR-based case reports in that it deals with panic attacks as the primary complaint. In both cases in this report, a therapy alternative to medication was necessary because the patients refused or were hesitant to take the medications prescribed by the hospitals that initially treated them due to the discomfort after intake and fear of substance dependence. This was despite the fact that they suffered not only from panic attacks, but also from symptoms related to anticipatory anxiety. Given that meditation is generally performed in orderly and calm environments, unpredictable situations such as panic attacks may be considered difficult to apply. In contrast, BCM applied in the described cases was verified to be efficient because its method of breath counting can directly help shortness of breath, one of the main symptoms of a panic attack. This method can be spontaneously applied in any urgent situations and during any activities7). The patients were instructed to count from one to ten at every exhalation using BCM in whatever body posture they were in;as a result, its effects in calming the symptoms of panic attack could be verified. While it is well-known that various meditation methods including BCM can reduce psychological anxieties and tensions, primary attention has been focused on the effects of continuous and disciplined meditation practice4) and no cases of spontaneous application of meditation to sudden symptoms such as panic attacks have ever been reported. Therefore, this case report is considered significant in that it presents the possibility of clinical application of BCM by different methods.
The efficacy of BCM is dependent on the total concentration on sensitizing the process of breathing. Breathing is an instinctive and involuntary bodily process, and in its pure sense, is not associated with desire or thought. Therefore, the BCM method using breathing is not complicated or abstract and easy to teach and practice, and thus, suitable for people without any meditation experience7). Desires and thoughts are by nature paradoxically resilient to attempts at controlling them and effacing them from the mind. Therefore, instead of indulging in a tug-of-war against such recalcitrant desires and thoughts, directing the attention away from them to the bodily senses is considered to prove more efficient in controlling them.
The comparison between BCM applied in this case report and MBSR applied in previous case reports reveals that MBSR centers on inducing an objective contemplation of “I” on one’s own behaviors, feelings, and thoughts while keeping the distance between “I” and the object. On the other hand, BCM focuses on sensitizing the breathing instead of contemplation, and thus, helps “I” empty the mind of desires and thoughts occupying it. This mind-emptying feature of BCM may also be useful in the practice of MBSR because BCM can help the MBSR meditator keep an objective distance from the object of contemplation instead of being attracted to the desires and thoughts arising in relation to specific circumstances. Furthermore, the simple method, enabling beginners to practice BCM without special training or exercise7), is also suitable as the first stage of MBSR in which the physical and mental senses and emotions encountered during meditation are accepted as they are and contemplated, thus helping patients achieve the therapeutic goals. Based on this, a variety of new and efficacious meditation programs tailored to specific needs can be developed.
As limitations of this report, it should be pointed out that an exclusive BCM therapy was not possible in these cases. Case 1 could not be followed up although positive therapeutic effects were found to be constant even during the last (fifth) visit after a month’s interval, and Case 2 could not be observed following therapy termination after 6 visits. Given that anxiety disorders usually have prolonged courses and varying outcomes12), continuous follow-ups are necessary including a follow-up study with a larger sample size and controls.
The following results were observed in the two cases after applying BCM for anxiety disorder treatment:
1. BCM significantly reduced the anxiety level in patients with a clinical anxiety disorder.
2. BCM can be effectively used for counteracting panic attacks appearing in a clinical anxiety disorder.
3. BCM has a potential to be efficiently used in the Korean Medicine psychiatry in combination with MBSR with mutually complementing effects.