Kaposi’s varicelliform eruption (KVE) is a cutaneous dissemination of viral infection in the setting of an underlying chronic skin condition. Particularly, the infection, which is caused by the herpes simplex virus (HSV), is called “eczema herpeticum”. Preceding skin conditions mostly include atopic dermatitis (AD) [1]. The number of reported cases of KVE has increased as the incidence rate of AD is still on the rise. The use of steroids or topical tacrolimus has been reported to be the main risk factor causing KVE in patients with AD [2, 3].
Also, patients are becoming aware that AD is a chronic skin disease that is recalcitrant to conventional Western treatments, and that the prolonged use of steroids may lead to various side effects. Therefore, many patients in Korea are willing to turn to alternative methods of treatment, especially Korean medicine (KM) [4].
Several case reports on the treatment of KVE with oral or intravenous antiviral therapies of Western medicine have been published [1, 5, 6], but no reports on the treatment of KVE with KM therapies, excluding Western medicine, have been published. As we successful
The patient was a 25-year-old male who has suffered with AD from infancy and who had temporarily recovered at the age of fourteen after a long period of continuous conventional treatments. No other medical history was seen except for allergic rhinitis. In August 2011, he had a right malleolus lateralis fracture and was admitted to a local orthopedics clinic. However, during the three weeks of admission, his skin condition was exacerbated after taking analgesic and antibiotic drugs every day. After that, he restarted conventional medication to alleviate the relapsed AD, but to no avail. On the 21st of December 2012, he experienced epigastric discomfort with mild fever, chills and fatigue after eating pork-boiled rice soup. The next day, rashes, pustules, vesicles and oozing abruptly appeared on his face and neck. On the 23rd, he was diagnosed in our clinic as having KVE and was hospitalized for a week. He did not take any conventional medication during whole process of the disease.
Herbal medicine,
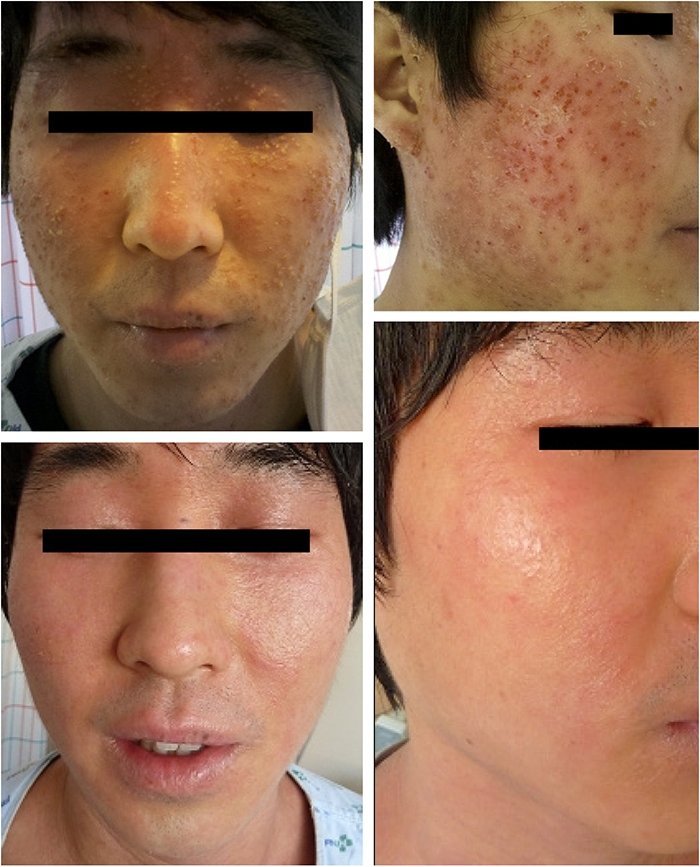
On the admission day, extensive vesicles and pustules, some of which had ruptured, oozed and crusted, appeared all over the face. The patient complained of a mild headache and a heat sensation on the face, but his vital signs were normal. Particularly, itching increased to the level of 4 on the numerical rating scale (NRS) during that nighttime while none had been seen during the day. The next day, the headache and the heat sensation totally disappeared. On the 4th day, most of the vesicles, papules, oozing and crust disappeared, but redness and scales still remained. Nighttime itching decreased to half, NRS 2. On the 7th day, facial redness and scales were all cleared. Itching almost disappeared, so he was discharged after a complete recovery (Fig 1).
Austrian dermatologist Moriz Kaposi gave the first description of KVE as a complication of infant eczema, which is characterized by widespread chickenpox-like vesicles superimposed on an underlying skin condition [7]. In 1941, Seidenberg suggested that the HSV was the primary cause of this disease [8]. The diagnosis of KVE is mainly clinical, but can often be delayed because KVE is easily mistaken for an aggravated skin condition of an existing disease.
KVE is clinically characterized by the sudden appearance of monomorphic, umbilicated, grouped vesiculopustular lesions on the face, particularly around the eyes, neck, axillae, chest and upper extremities. The eruption is usually accompanied by fever and regional lymphadenopathy. Generally, the localized type of KVE heals naturally without permanent scarring; however, the systemic type of KVE can be fatal.
An impaired barrier function of the epidermis and an immunological abnormality have been proposed as causes for the development of the infection [9]. Especially, the suppressed function of T cells causes AD patients to become vulnerable to viruses [10], as increased IL-4 secreting cells in the lesion interrupt the immune reaction to HSV by inhibiting Th-1 cell activity [11]. Furthermore, KVE has been thought to occur due to decreased levels of IL-18, which is known to have profound influences on the pathological conditions of immune diseases [12]. Skin lesions of AD are often damaged by scratching and can spread to their surroundings because HSV is commonly found even on unaffected regions, such as both hands [13]. However, KVE does not always follow a preceding eczematous skin disease [14], and sometimes refers to an extensive infection of HSV in patients with decreased immunity. Taken altogether, the exact pathogenesis of KVE remains to be elucidated.
Tacrolimus, an immunosuppressant widely used for treating AD, is known to cause disruptions in the topical skin immune system, finally leading to secondary infections [15]. Also, Stroud [16] reported that large amounts of steroids proportionately increased the severity scale of HSV.
Kim
The authors mixed HP and 25% BVP solutions as a main intervention in this case. The antiviral effect of mellitin, a main component of BVP, has been suggested in several research reports [18, 19], to play a key role in inhibiting viral activities, even those of HIV. To relieve the inflammatory responses caused by the virus, we selected HP, which is a typical antiphlogistics in KM. Various articles [20, 21] have reported on its proven anti-inflammatory effects and mechanisms. Selected acupoints, both BL13, are relevant to the lung, which governs the skin system.
The herbal medicine,
Sama Upper, Middle and Lower of Master Tung acupuncture is used to treat skin diseases [23] and ST44 eliminates heat sensation of the face [24].
KVE is an acute, life-threatening, exigent skin disease. This case is significant in that an acute skin infection was completely cured with KM alone. In conventional Western medicine, the localized type of KVE can be cured within 7 to 10 days, on average, if antiviral agents are properly administered [4-6]. That viral disease can be treated with complementary and alternative medicine (CAM) methods in the same amount of time is meaningful, and if CAM is combined with conventional medicine, better control of more severe viral diseases can be expected. However, this case is only one case of mixed therapies, so more case studies will be needed.