Aripiprazole is unique drug among the second- generation antipsychotics in its pharmacology and pharmacokinetics, but is similar in clinical efficacy 1). Aripiprazole acts as a partial agonist at dopamine D2 receptors, activating the receptor but eliciting a reduced response compared to the natural neurotransmitter. The drug is also a partial agonist of serotonin 5HT1 a receptors, but an antagonist of 5HT2a, H1, and alpha-1-adrenergic receptors.
While both first- and second-generation antipsychotics have been used as maintenance therapy to prevent relapse in patients with stable schizophrenia, atypical antipsychotics have better tolerability profiles, including a lower risk of extrapyramidal symptoms (EPS)2,3). The atypical antipsychotic agents, which include amisulpride, aripiprazole, clozapine, olanzapine, quetiapine, risperidone, sertindole, ziprasidone, and zotepine have greater efficacy in terms of symptoms of schizophrenia compared with that of first-generation antipsychotics.
The most common side effects of aripiprazole are headache, nausea, vomiting, insomnia, tremor, and constipation. Weight gain has been minimal in short and long-term trials. The drug has shown a lower risk of EPS, increases in lipid or prolactin levels, and sedation, compared to other atypical antipsychotics in a small number of comparative trials 4). It has not been found to cause QT prolongation.
Clinical trials of adults with schizophrenia started the drug at 10∼15 mg daily, administered in a single dose. This dose proved to be adequate for many patients, but doses up to 30 mg daily have been approved. The manufacturer’s clinical trials for bipolar disorder started patients at 30 mg daily and lowered the dose only for side effects. Studies in the elderly population have not been reported, but expert opinions suggest doses of 15∼30 mg daily in elderly patients with schizophrenia5).
Difficulty in opening the eyes is not yet defined as an EPS; however, it is a rare but important side-effect of aripiprazole. In this report, we discuss a case of difficulty opening the eyes during aripiprazole therapy.
The case was a 26-year-old single female of South Korean ethnicity suffering from paranoidtype schizophrenia with auditory hallucinations diagnosed when she was 20 years old. She visited a Korean psychiatric clinic due to difficulty in opening her eyes. When the patient first visited the clinic, she did not appear to be depressed, and could open her eyes 5 min after she woke up and after a short sleep. However, she was almost unable to open her eyes by using her hands to hold up her eyelids on the first day. The patient did not have a heavy feeling on her eyelids, but if somebody held her eyelids, there was a feeling of needing to shut her eyes, so she could not keep her eyes open. It was easier for the patient to open her eyes when she was lying in bed.
The patient first experienced hallucinations at 20 years of age, as she sensed that somebody cursed at her from nearby lockers. After this incident, she visited the psychiatric clinic and was administered an antipsychotic. The physician prescribed a 4-week course; however, the patient stopped the medication after 1 week because she confirmed that no-one was present beside the lockers.
The patient’s father was diagnosed with schizophrenia and was repeatedly treated in a closed ward. He had delusions, talked to himself, and liked to talking with an imaginary person. For this reason, her parents were divorced when she was 14 years of age.
As a university student, the patient was lonely because she argued with friends. When a group of friends discussed the theme of a project, she was excluded from the meeting. The patient felt as though she were an invisible person.
Two years before coming to the Korean psychiatric clinic, the patient had a delusion and again began taking the antipsychotic. She had fallen in love with someone who did not love her?indeed, the person did not know her. However, she thought that he loved her. One day, the patient said to her mother “Did you tell him something bad about me?” The same thing happened to both her friend and her elder sister. Therefore, a friend of the patient doubted her sanity, and suggested a visit to a psychiatric clinic. The patient then visited a psychiatric clinic and was taking an antipsychotic
until 4th September.
While taking the antipsychotic, the patient gained weight and developed hypersomnia and tonic walking, similar to a robot. For this reason, the physician changed the antipsychotic repeatedly from aripiprazole to paliperidone, and then to aripiprazole again.
On 4th August, she was admitted to a psychiatric clinic at the university hospital to treat the symptom of “Eyelids falling automatically”; this differed from ptosis. An electromyogram, Jolly’s test, and a repetitive nerve stimulation test (RNST) were performed on the right oribicularis oculi, abductor digiti minimi, and flexor carpi ulnaris. The RNST revealed no electrophysiological evidence of a neuromuscular junction disorder. At this time, she had been taking 30 mg aripiprazole per day for 1 month. The patient was discharged from the hospital after 20 days, at which time she could open her eyes.
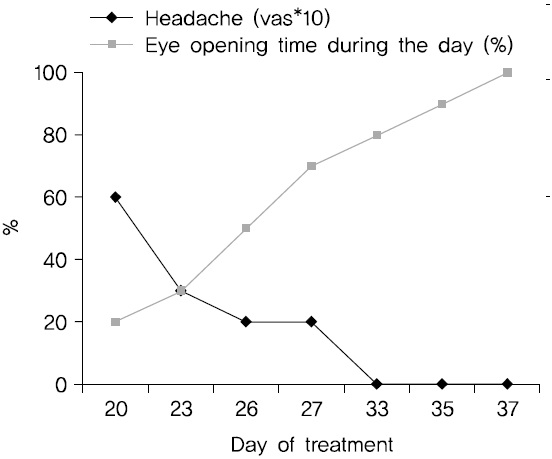
The same symptoms occurred 10 days later. The patient visited the Korean psychiatric clinic. During hospitalization, she was treated with electroacupuncture on an eye-related acupoint and herbal medicine, which facilitates detoxification. The patient’s symptoms improved after relaxation therapy was focused on closing her eyes comfortably. When the patient first closed her eyes, the eyeballs wobbled. After 1 week, the eyeball wobble improved significantly, and headache pain decreased (Fig. 1).
Aripiprazole-related problems, such as acute laryngeal dystonia6), tardive dyskinesia, and dystonia have been reported. The difference is that previous reports pertained to the lips, tongue, jaw, and neck (torticollis)7-10), but difficulties opening the eyes due to tension in the eyelid have not been reported. Our patient visited another hospital before coming to the Korean psychiatric clinic, where conversion disorder was diagnosed. However, this was different from conversion disorder. Conversion disorder causes patients to suffer apparently neurological symptoms, such asnumbness, blindness, paralysis, or fits, but without a neurological cause. These symptoms are thought to arise in response to difficulties in the patient’s life, and conversion is considered a psychiatric disorder. Psychological factors were judged by the clinician to be associated with the symptom or deficit because conflicts or other stressors preceded their initiation or exacerbation. She had taken a teacher certification examination 2 years prior, but the initiation differed in that when she was under stress, she could not open her eyes.
Numerous studies have reported mechanisms of acute dystonia related to dopamine hypofunction, resulting in relative overactivity of cholinergic mechanisms. As aripiprazole lacks protective anticholinergic action, it can precipitate dystonia. This is supported by the fact that the dystonia resolved with administration of promethazine (an antihistaminic with an anticholinergic property) in this case. In addition, the action of aripiprazole on the D3 receptor and antagonism of 5-HT6 and 5-HT7 receptors remains unknown, and, hence, it may play a role in oculogyric dystonia. Preclinical studies have reported an inhibitory action of aripiprazole on the serotonin transporter, which may alter the dopamine balance in the basal ganglia region. Some studies have reported paradoxical dopaminergic hyperfunction by either preferentially blocking presynaptic receptors or exposing the postsynaptic receptors to the natural release of dopamine from the presynaptic terminals as DBA levels drop, which may result in dystonia9).
It is important to recognize aripiprazole-related oculogyric dystonia early to prevent life-threatening complications. Educating medical staff regarding this easily treatable reaction will improve the overall quality of healthcare. This case emphasizes the need for awareness of the risk for acute oculogyric dystonia in adolescent female patients receiving aripiprazole.
Korean special therapy is effective for treatment of this symptom. Relaxation therapy not only reduces tension in the eyelids, but also ameliorates headache symptoms. At the same time as it was becoming easier for our patient to open her eyes, her headaches also decreased. If a patient cannot open their eyes because of tension, it is more useful to teach them not to open their eyes but to try to close them using little force on the eyelids. Therefore, relaxation therapy is an important component of treatment of the side effects of atypical antipsychotics.