of the spinal canal, lateral recess and intervertebral foramen. It causes ischemia to the nerve roots or cauda equina by narrowing of the neural tube, leading to neurological symptoms [1]. The L4-5 spinal disc is most frequently affected, and the most common ages for the on set of spinal stenosis lateral recess and foraminal stenosis, as well as the centrality common, are the 50s and the 60s [2].
Most of spinal stenosis is degenerative spinal stenosis caused by degenerative changes in the disc, and facet joints reduction in the height of the degenerative disc, spur formation, thickening of the ligaments flava and the central spinal canal, and narrowing of the lateral recess and foramen. Also it can be caused by spondylolisthesis [3]. Intermittent neurogenic claudication is the most common symptom of lumbar spinal stenosis. Also, low back pain, lower limb radiating pain, paresthesia and weakness of the hip or thigh are symptoms of spinal stenosis [4]. These symptoms are improved during lumbar delordosing and reduced during the rest [5].
Acupotomy is one of the acupuncture treatment methods. It is performed at the same time as needles and mes. It has better therapeutic effect than regular acupuncture and has the advantage of quick recovery and pain reduction compared to Western medicine and surgery therapy [6]. Because of these advantages, acupotomy is widely used in many kinds of muscular diseases such as herniated inter vertebra disc (HIVD) of lumbar spine [7].
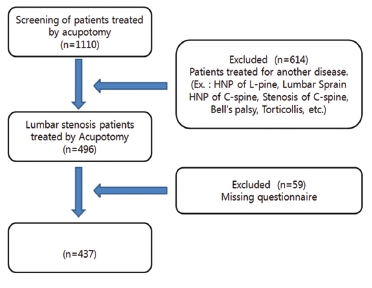
Despite the overall effectiveness of acupotomy, the effect of acupotomy on lumbar spinal stenosis has been less studied. Therefore, this study included a total of 437 patients who had been diagnosed with lumbar spinal stenosis and who had undergone acupotomy from June 1, 2008, to September 31, 2012, and used the verbal numeric rating scale (VNRS), the oswestry disability index (ODI) and global assessments to investigate the effect of acupotomy on lumbar spinal stenosis.
A total of 437 patients who had been diagnosed with lumbar stenosis from June 1, 2008, to September 31, 2012, by using magnetic resonance imaging (MRI) and for whom surgery had been recommended participated in this study. Participants were admitted to Daejeon Oriental Hospital. Oriental treatment and acupotomy were treated in parallel, and patients underwent acupotomy from one to three times depending on the degree of stenosis and their physical condition (Fig 1)
2.2. Treatment methods before and after acupotomy
After admission, participants took acupuncture twice a day and acupotomy once a day using 0.25 × 0.30 ㎜ and 0.35 × 0.50 ㎜ stainless-steel disposable acupuncture needles (Dongbang, Korea). According to participants symptoms and acupuncture points, the needle depth was about 10-20 ㎜ or 30-40 ㎜, and the needles remained in place for about 15-20 min. In addition to acupuncture treatment, interferential current therapy (ICT), hot pack, herbal medicine, moxibustion and cupping were used to improve muscular relaxation and blood flow, and manual therapy was performed once a day.
articipants were fully informed of the side effects and contents of the pre-surgical procedures, and written informed consent was obtained from the participants before acupotomy. Anes Cream (Teaguk, Korea) 2EA was applied to lower back of every participants one hour before acupotomy for local anesthesia. Also participants took acetaminophen (Samnam, Korea), one tablet, to relieve pain during acupotomy. The lower back where acupotomy was performed was sterilized in advance. A flat-head-screwdriver-shaped 1.0 × 75 ㎜ stainless-steel disposable acupuncture needle (Dongbang, Korea) was used in acupotomy. After the depth from the skin to the ligament flava had been measured using actual-sized X-ray, the needle was inserted between the spinous process and stimulated the ligament flava. Also, needles was inserted 20 ㎜ - 30 ㎜ apart on both sides of the spinous process and stimulated erect the spinae and the intertransverse ligament which surrounds the facet joint. According to participants, the depth was about 60 - 70 ㎜. During the acupotomy, the practitioner checked the participant’s pain, and no numbness due to nerve damage was observed. The acupotomy site was sterilized, after which sterilized gauze was applied to the site. Participants took admission treatment at least one day after acupotomy. Acupotomy was performed from one to three times depending on the degree of stenosis and the physical condition of the participants.
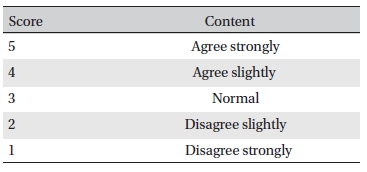
To evaluate the effect of acupotomy, we used three measurement instruments before and after acupotomy: the VNRS, the ODI, and a global assessment. The VNRS is one of the most commonly used pain scales. In numeric scales, patients verbally score their pain from 0, indicating the absence of pain, to 10 indicating the most intense pain possible [8]. The ODI is one of the principal condition- specific outcome measures used in the management of spinal disorders. The ODI, which was made by Fairbank, is comprised of 10 items, including standing, walking, sitting, bending etc. Each of the 10 items is scored from 0 to 5, so the maximum number of points is 50 [9]. The global assessment was designed to investigate the overall satisfaction with acupotomy. Global assessment grades ranged from 1 to 5, with grade 1 indicating disagree strongly, grade 2 indicating disagree slightly, grade 3 indicating normal, grade 4 indicating agree slightly, and grade 5 indicating agree strongly (Table 1)
We statistically analyzed demographic data and we present quantitative data as means ± standard deviations. To evaluate the effect of acupotomy, we used the paired
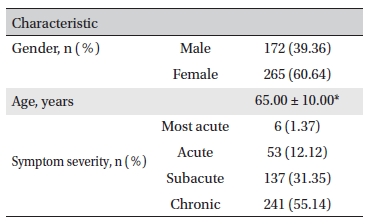
Among the 437 participants, 172 men and 265 women participated in this study, and gender ratio of 1:1.54. Ages ranged from 38 yr old to 94 yr old. The mean age was 65 ± 10.0 yr. Among the 437 participants, 190 participants were under the age of 65, and 247 participants were over the age of 65, a ratio of 1:1.3. The period of disease was classified into four groups. A period of one week after onset was most acute, a period from one week to one month after onset was acute, a period from one to six months after onset was subacute, and a period of more than six months after onset was chronic. Six participants were classified as the most acute, 53 as acute, 137 as subacute and 241 as chronic. The average period of the disease was 30.17 ± 56.63 months (Table 2)
Global Assessment
[Table. 2] Characteristics of the study subjects
Characteristics of the study subjects
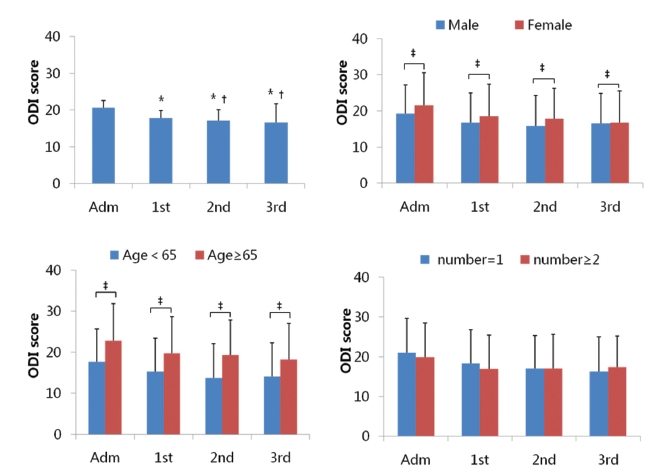
All particpants’ VNRSs on admission were 10. After the 1st acupotomy, the VNRS decreased to 7.10 ± 2.50, after the 2nd acupotomy, the VNRS decreased to 6.30 ± 2.60, and after the 3rd acupotomy, the VNRS decreased to 5.50 ± 2.50. All particpants’ average ODI score on admission was 20.60 ± 8.70. After the 1st acupotomy, the ODI score decreased to 17.80 ± 8.60, after the 2nd acupotomy, the ODI score decreased to 16.70 ± 8.60, and after the 3rd acupotomy, the ODI score decreased to 5.50 ± 2.50. The global assessment was 3.70 ± 0.70 after the last acupotomy (Figs 2,3)
The ODI scores on admission were found to have a statistically significant impact on the ODI scores after the 1st, 2nd, and 3rd acupotomies (
There were statistically significant differences between the VNRSs after the 1st and the 2nd acupotomies, the VNRSs after the 1st and the 3rd acupotomies, and the VNRSs after the 2nd and the 3rd acupomtomies (
For men, the ODI score on admission was 19.20 ± 8.00. After the 1st acupotomy, the ODI decreased to 16.80 ± 8.10, after the 2nd acupotomy, the ODI decreased to 15.90 ± 8.30, and after the 3rd acupotomy, the ODI decreased to 16.60 ± 8.20. For women, the ODI score on admission was 21.60 ± 9.00. After the 1st acupotomy, the ODI decreased to 18.50 ± 8.90, after the 2nd acupotomy, the ODI decreased to 17.80 ± 8.50, and after the 3rd acupotomy, the ODI decreased to 16.80 ± 8.80. For men, after the last acupotomy, the global assessment score was 3.70 ± 0.70; for women, it was 3.70 ± 0.80. The gender differences in the ODI scores between admission day and the 1st, 2nd, and 3rd acupotomies were statistically significant (
Under the age of 65, after the 1st acupotomy, the VNRS decreased to 7.00 ± 2.50, after the 2nd acupotomy, the VNRS decreased to 5.00 ± 2.70, and after the 3rd acupotomy, the VNRS decreased to 5.00 ± 2.60. Over 65 yr of age, after the 1st acupotomy, the VNRS decreased to 8.00 ± 2.50, after the 2nd acupotomy, the VNRS decreased to 7.00 ± 2.60, after the 3rd acupotomy, the VNRS decreased to 5.00 ± 2.50.
Under the age of 65, the ODI score on admission was 17 ± 8.00. After the 1st acupotomy, the ODI decreased to 15.30 ± 8.10, after the 2nd acupotomy, the ODI decreased to 13.80 ± 8.30, and after the 3rd acupotomy, the ODI decreased to 14.10 ± 8.20. Over 65 yr of age, the ODI score on admission was 22.80 ± 9.00. After the 1st acupotomy, the ODI decreased to 19.70 ± 8.90, after the 2nd acupotomy, the ODI decreased to 19.30 ± 8.50, and after the 3rd acupotomy, the ODI decreased to 18.20 ± 8.80.
Under the age of 65, after the last acupotomy, the global assessment score was 4.00 ± 0.80, and it was 3.80 ± 0.7 for participants over 65 yr of age. The differences in the ODI scores for the two age groups between admission day and the 1st, 2nd, and 3rd acupotomies were statistically significant (
For stenosis by more than 2 parts, the ODI score on admission was 19.90 ± 8.60. After the 1st acupotomy, the ODI decreased to 16.90 ± 8.50, after the 2nd acupotomy, the ODI decreased to 17.10 ± 8.50, and after the 3rd acupotomy, the ODI decreased to 17.40 ± 7.80. For one part stenosis, the ODI score on admission was 21.00 ± 8.60. After the 1st acupotomy, the ODI decreased to 18.30 ± 8.50, after the 2nd acupotomy, the ODI decreased to 17.00 ± 8.30, and after the 3rd acupotomy, the ODI decreased to 16.30 ± 8.70. For stenosis by more than 2 parts, after the 1st acupotomy, the VNRS decreased to 6.90 ± 2.50, after the 2nd acupotomy, the VNRS decreased to 6.30 ± 2.70, and after the 3rd acupotomy, the VNRS decreased to 5.20 ± 2.50. For one part stenosis, after the 1st acupotomy, the VNRS decreased to 7.30 ± 2.50, after the 2nd acupotomy, the VNRS decreased to 6.30 ± 2.70, and after the 3rd acupotomy, the VNRS decreased to 5.70 ± 2.60. For stenosis by more than 2 parts, after the last acupotomy, the global assessment score was 3.80 ± 0.70, and it was 3.70 ± 0.80 in the case of one part stenosis. The differences in the ODI scores, the VNRSs, and the global assessments between stenosis-number group were not statistically significant (Figs 2,3)
Lumbar spinal stenosis is a disease that causes a variety of complex neurogical symptoms, such as back pain or lowerlimb pain, caused by a narrowing of the spinal canal, the nerve root canal or the foramen [10]. The problem of congenital spinal symptoms may occur at a young age. However, most of the stenosis caused by degenerative changes mainly occur in patients in their 50s to 70s [11]. Spinal stenosis is caused by thickening of the facet joint, overlapping or thickening of the ligament flavum, lumbar disc herniation, and spinal degenerative spondylolisthesis [12]. Neurogenic claudication and leg pain are the main symptoms of spinal stenosis. Typically neurogenic claudication appears when cauda equina press is caused by central stenosis. Sciatica or leg pain appears when the nerve root compression is caused by foraminal stenosis [13, 14]. When conservative treatment is not sufficient, surgical treatment should be considered. Surgical therapy is performed when cauda equina syndrome and severe peripheral nerve symptoms, especially muscle weakness, interfere with day life because of severe neurological claudication [15].
Recently, in Oriental medicine, acupuncture clinical therapy has been improved. In addition to traditional acupuncture therapies have been used in the treatment of spinal stenosis [16], but the effect of acupotomy treatment for spinal stenosis has not been studied yet. Thus, 440 participants who underwent acupotomy were studied to determine the effect of acupotomy treatment for stenosis. The results are as follows;
In this study, the VNRSs and the ODI scores were significantly decreased, which means that acupotomy as a treatment for spinal stenosis has a significant effect on pain relief and functional recovery of every day life. The global assessments were high enough to suggest that the majority of the participants were satisfied with acupotomy. Also, for men under 65 yr of age, a higher improvement can be expected, and the symptoms are expected to be improved when acupotomy lasts for up to three times. However, in this study, there was a difference in the gender ratio of patients, the number of acupotomies was not constant per patient, ranging from one to three times, and the intervals between acupotomies were also slightly different, depending on the patients’ conditions. These are a few limitation of this study. Also, in this study, participants took other treatments, such as physical therapy, moxibustion therapy, drug therapy, and cupping therapy. These treatments were carried out uncontrolled conditions, so it is not certain whether acupotomy was independently effective or not. In this study, there were no control group, and this was not a prospective, long-term study. Therefore, further studies are needed.
This study’s results show that acupotomy is good for the treatment of lumbar stenosis. This means that acupotomy is significantly effective for reducing stenosis patient’s symptoms, such as pain, claudication and so on. Furthermore acupotomy is a good treatment therapy for improving patient’s quality of life. Continued research is thought to be needed to further increase the effectiveness of acupotomy. Long-term follow up studies are also needed.