Pharmacopuncture, or herbal acupuncture, is a new form of therapy derived from combinations of two traditional therapeutic methods, herbal medicine and acupuncture therapy. In general, pharmacopuncture treatment is performed by injecting small amounts of extracted medicinal materials at acupuncture points or in affected areas in order to combine the efficacies of the acupuncture and the drug [1]. Although the first primitive trials with bee venom or herbal extractions were recorded in old medical books from the Han Dynasty of China, acupuncture with injection started in the early 1950s in China and was referred to as aquapuncture [2,3]. Recently, pharmacopuncture has been adopted with success in Korea and has developed into quite a unique and systematic framework for the diagnosis and treatment of various diseases [4]. Most researchers have focused on specific types of pharmacopuncture for the treatment of specific types of diseases.
The purpose of the present study was to evaluate the efficacy of Geumgoeshingi-whan (GGSGW) Pharmacopuncture in the treatment of elevated blood pressure. In addition, we investigated whether the effects of the GGSGW Pharmacopuncture on the blood pressure were influenced by renal fluid and electrolyte handling.
The experiment was conducted on male spontaneously hypertensive rats (SHR) weighing approximately 250 g. None of the rats had any clinically evident infections. The animal room was controlled for temperature (23 ± 2°C), humidity (50 ± 10%) and light (12 h light-dark cycle). The animals had free access to rat chow and tap water ad libitum for two weeks. All animal care and experimental procedures described in this study were in compliance with the protocols dictated by the Animal Care Committee of Wonkwang University.
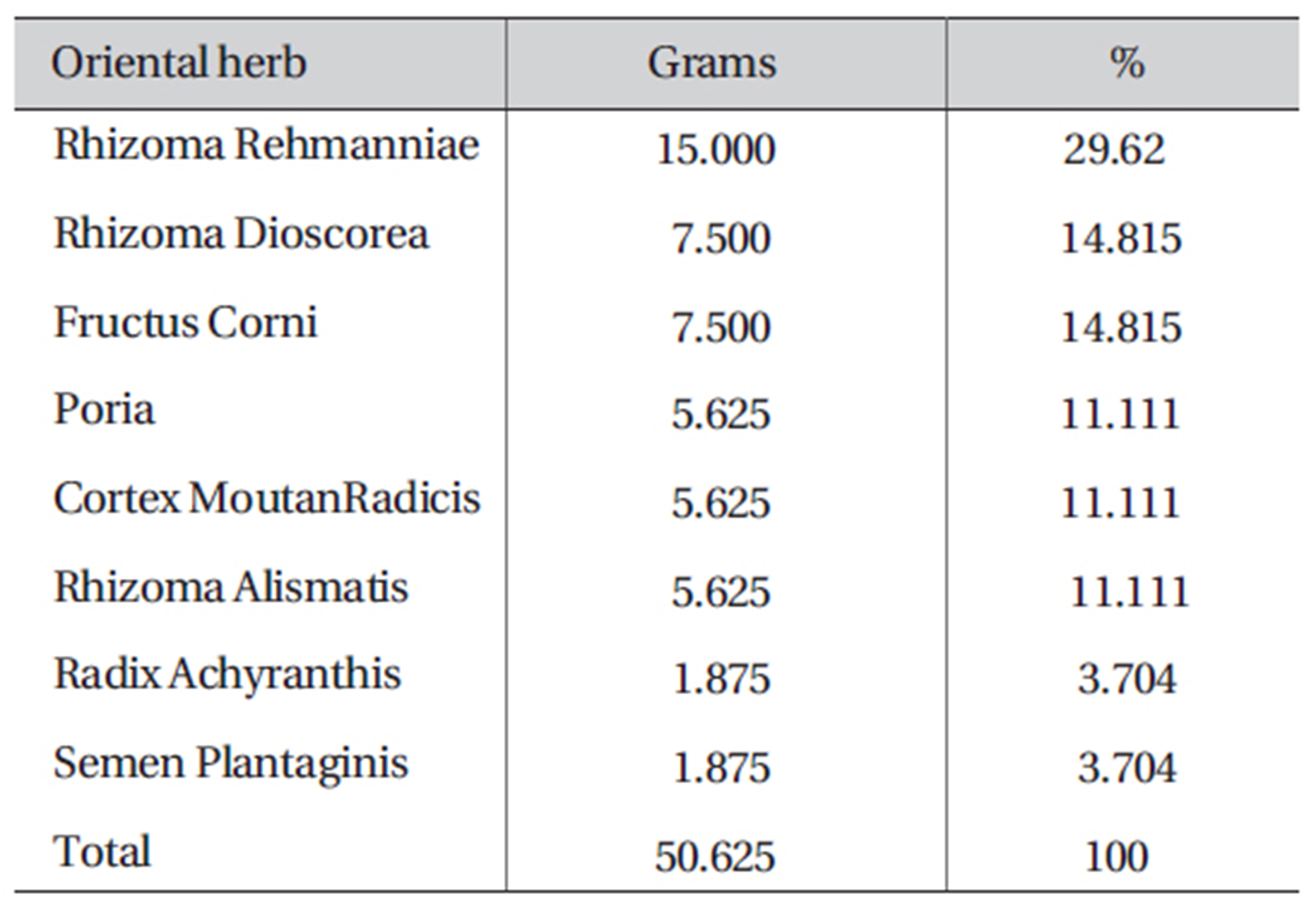
2. 2. Geumgoeshingi-whan (GGSGW) Pharmacopuncture preparation
The GGSGW Pharmacopuncture contains eight oriental medicinal herbs (Table 1). The herbal ingredients were obtained from the Oriental Medical Hospital of Wonkwang University (Gwangju, Korea). The water based extract was prepared as follows: The dried, pulverized medicinal herbs were mixed together and each 253.1g batch was soaked with ultra pure water (800 ml) at room temperature for 80-90 min. After the leaching process, it was boiled in water at 100-107℃ for 120 min. After the boiling process, the vapor was condensed. After condensation the liquid was stored in a Freeze Dryer at - 30-40℃ for 1 day to remove any water. 460 mg of the resulting precipitate was used to make 0.9% isotonic GGSGW solution, pH 7.25-7.35. The liquid was placed in 10 cc vials and sterilized for 30 min by using high-pressure sterilizer equipment. The completed pharmacopuncture was stored in the refrigerator until it was used.
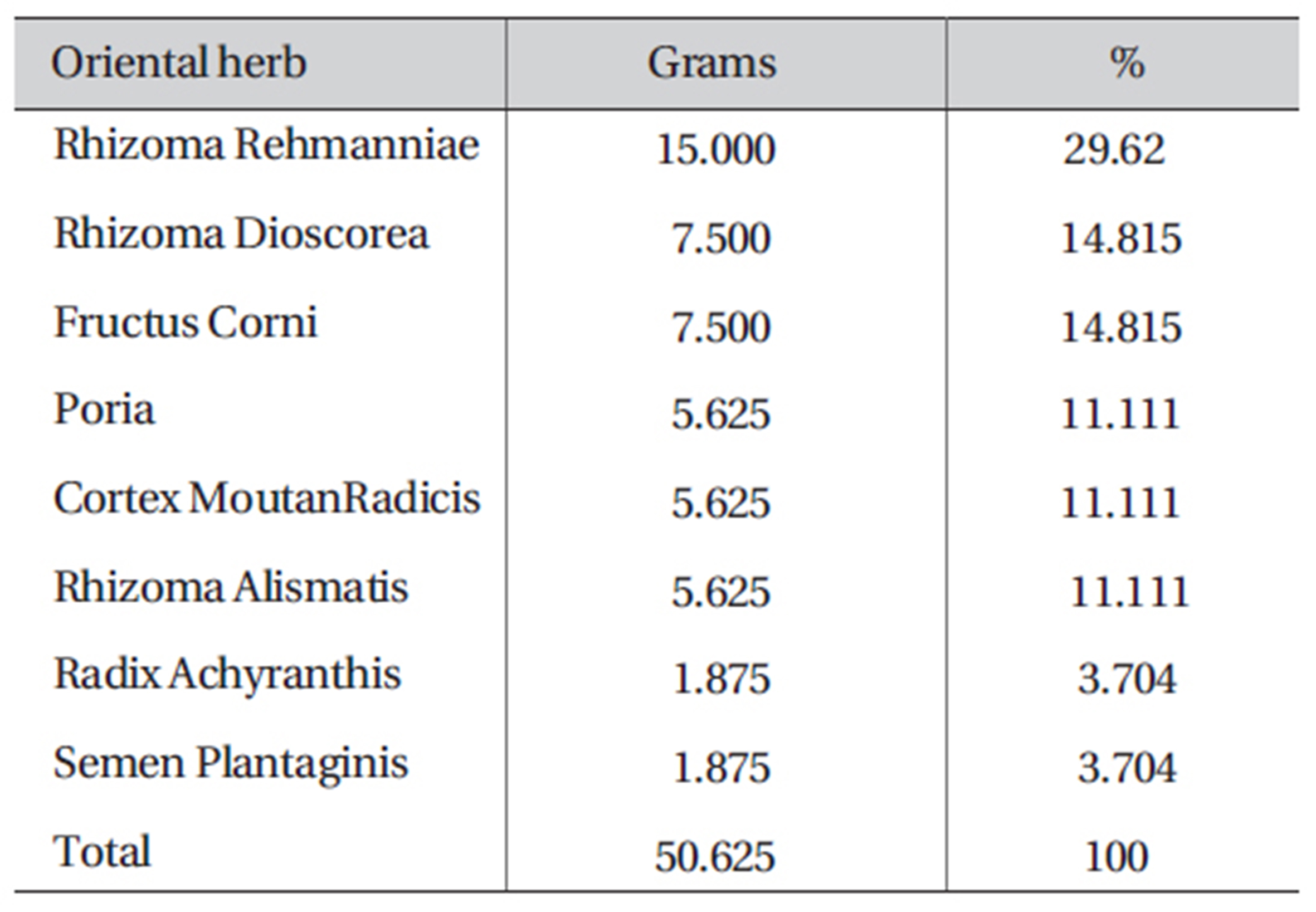
The composition of GGSGW
Spontaneously hypertensive rats (SHR) were injected with normal saline solution (Control-SHR group, n = 8) or GGSGW Pharmacopuncture (GGSGW-SHR group, n = 8). For the injections, 26-gauge safti syringes (Becton Dickinson Korea, Inc., Seoul, Korea) were inserted to a depth of 2-3 ㎜ at one day intervals for two weeks. The injected acupoint was Mingmen (GV 4) on the lumbar region. The anatomical location of the stimulated acupoint in the rats was determined in accordance with other reports [5].
2. 4. Blood pressure measurement
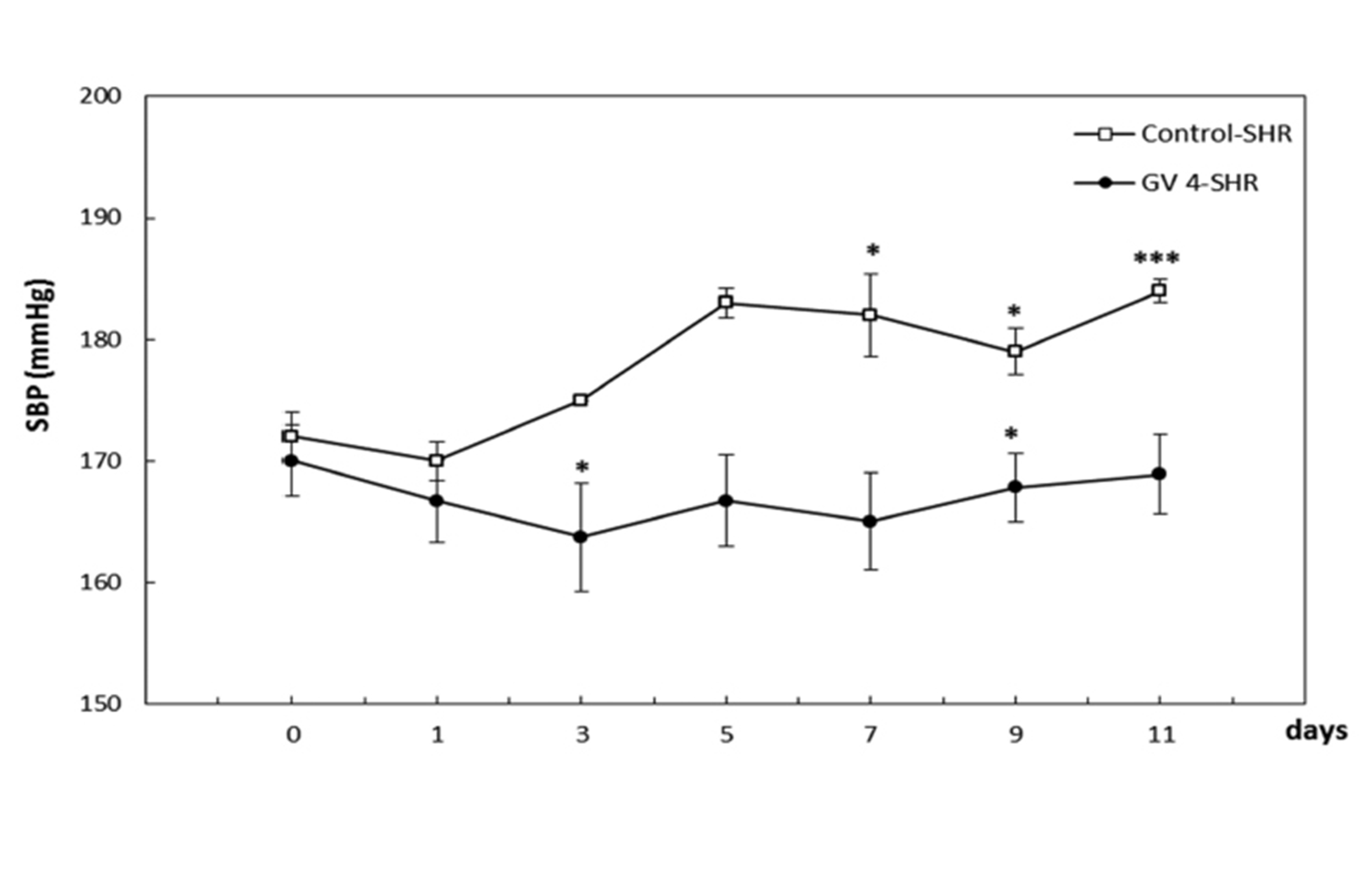
Measurements were taken every two days during the 2- week study to determine the effect of GGSGW Pharmacopuncture on the blood pressure. Measurements were performed on rats at the same time of day by the same researcher in random order. The systolic blood pressure (SBP) was measured under conscious conditions by use of the tail-cuff method with an electrosphygnomanometer. Before the rats were killed, the mean BP was measured by cannulation of the tail artery by using a Brush transducer and model 2200 recorder (Gould). The diastolic blood pressure (DBP) values were not collected because reliable DBP values are not obtained with the method used. If the rat was restless and no solid recordings were obtained, the measurement was stopped and repeated later.
2. 5. Urine and plasma analysis
Plasma and urinary creatinine concentrations were measured enzymatically (Creatinine PAP; Biocon Diagnostics) either in a spectrophotometer or a Roche Modular P analyzer (Roche Diagnostics). Plasma and urinary concentrations of sodium and potassium were measured by using flame photometry. Urine and plasma os molalities were determined using a micro-osmometer (Fiske). Aldosterone was measured by using an aldosterone solid-phase RIA kit (Diagnostic Products Corporation, Los Angeles, CA, U.S.A.). The concentration of atrial natriuretic peptide (ANP) in perfusates was measured using a specific radioimmunoassay, as described previously [6]. The molar concentration of ANP in terms of the Extracellular fluid (ECF) translocation reflects the concentration of ANP in the interstitial space of the atrium and, therefore, indicates the rate of myocytic release of ANP into the surrounding paracellular space [7]. Therefore, the molar concentration of ANP release in the interstitium was calculated as follows:
All values are presented as means ± SEMs (the small standard errors of the means, SE). Statistical analysis was performed using ANOVA for repeated measurement to investigate differences in time in each group and between treatments. Differences of
As shown in Fig 1, the SBP was gradually and significantly increased in the Control-SHR group while it was significantly attenuated in the GGSGW-SHR group compared to the Control-SHR group.
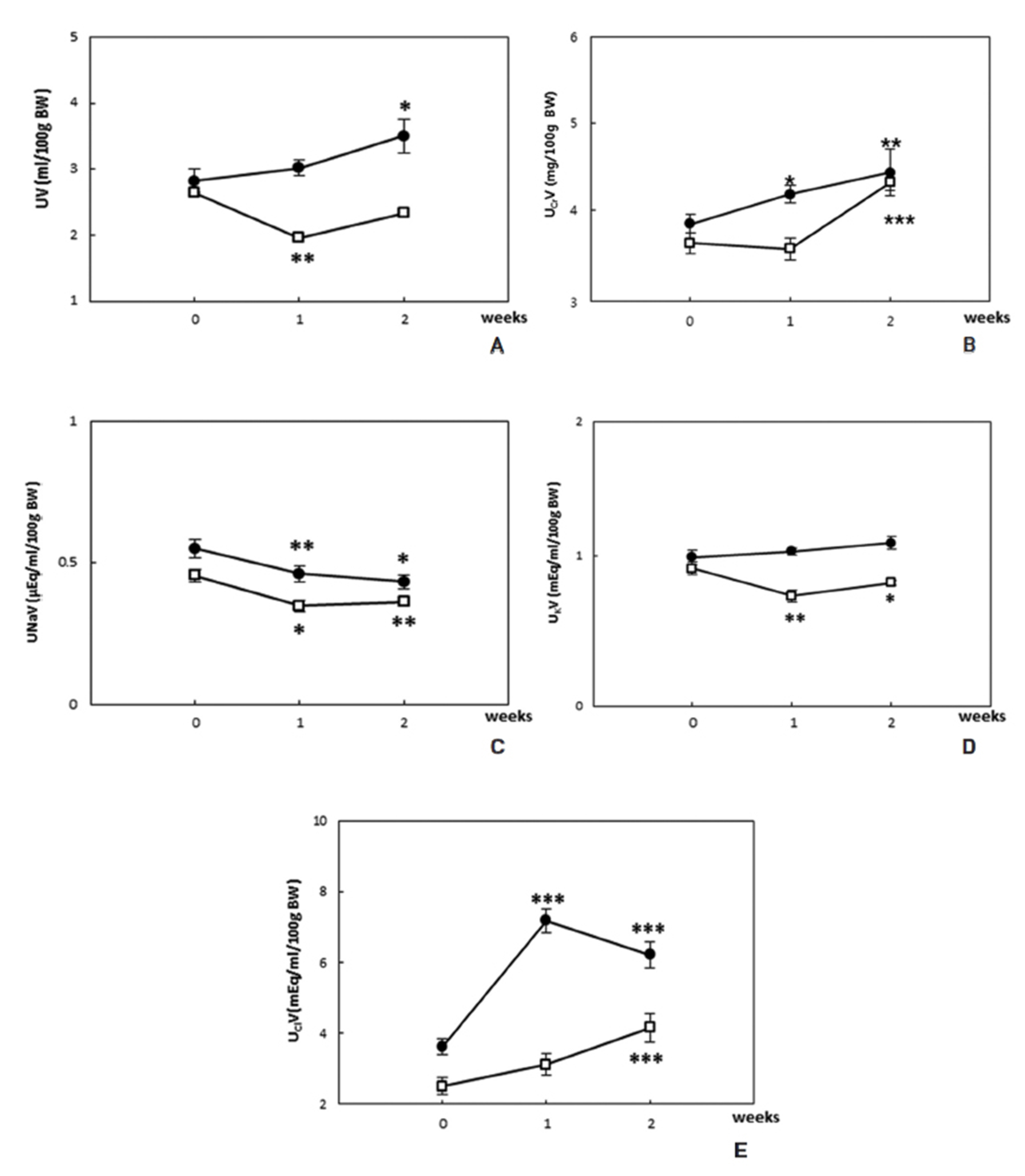
The renal parameters in the SHR administered GGSGW Pharmacopuncture are shown in Fig. 2 (A-E). The urine volume of the GGSGW-SHR group was significantly higher than that of the Control-SHR group. Creatinine clearance, as a measure of glomerular function, was also significantly higher in the GGSGW-SHR group compared with the Control-SHR group. The significant electrolytes in the GGSGW-SHR group were significantly higher than those in the Control-SHR group. Urinary sodium excretion was significantly decreased in both the GGSGW-SHR group and the Control-SHR group throughout the experimental period. Urinary potassium excretion gradually increased in both groups, but the change was not statistically significant. Urinary chloride excretion was significantly elevated in the Control-SHR group for the experimental period whereas urinary chloride excretion in the GGSGW-SHR group was lower after the first week of the experiment.
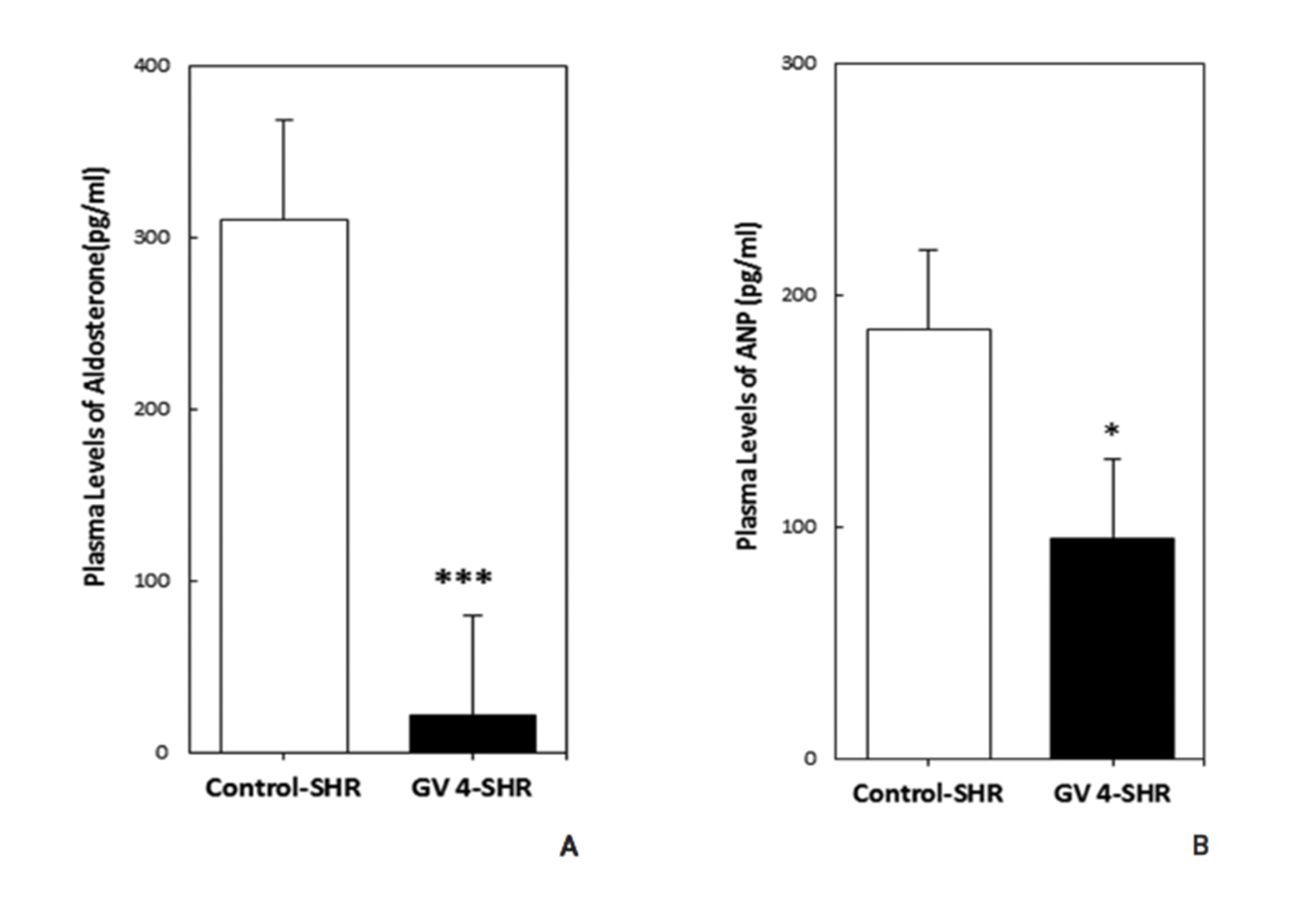
The plasma levels of ANP were also significantly decreased in the GGSGW-SHR group compared to the Control-SHR group (Fig. 3).
The salient findings of the present study suggest that the application of the GGSGW Pharmacopuncture to SHR caused a sustained decrease in arterial blood pressure and improved renal function, such as creatinine clearance, throughout a two-week study. The decrease in the SBP in SHR after administration of the GGSGW Pharmacopuncture (Fig. 1) was associated with a supposed fall in the plasma levels of aldosterone (Fig. 3). The present study also demonstrated that GGSGW Pharmacopuncture caused a marked decrease in the plasma levels of aldosterone and ANP. The possible mechanism by which the plasma ANP levels were decreased in the GGSGW-SHR group may be a systolic blood pressure-lowering effect of GGSGW Pharmacopuncture. An important stimulator of ANP release is hypertension [8], which was regulated by the physiological role of the GGSGW Pharmacopuncture. This effect on the plasma ANP levels could explain the hypotensive response observed after administration of the GGSGW Pharmacopuncture in the current study. The precise mechanism underlying the decrease in the arterial pressure induced by the GGSGW Pharmacopuncture has not yet been identified. The control of arterial pressure is thought to be dominated by renal control of fluids, electrolyte balance, and aldosterone.
In traditional Korean medicine, the etiology of hypertension is associated with qi deficiency in the kidney [9]. Other etiologies are ascendant hyperactivity of liver yang (a pathological change in which deficient liver-kidney yin lets liver yang get out of control and stir upward) [10], disharmony of qi and blood (any failure in the mutually coordinating relationship of qi and blood) [10], static blood (a pathological product of blood stagnation, including extravasated blood and blood circulating sluggishly or blood congested in a viscus, all of which may turn into a pathogenic factor, the same as blood stasis or stagnant blood) [10], phlegm-turbidity (a pathological change characterized by impairment of diffusion) [10], and so on.
The treatment focuses on supplementing warmth, by using methods that converge lower energizers, warming and toning the kidney qi, strengthening the kidney, harmonizing and complementing the kidney and the heart, complementing and promoting the kidney, and strengthening the liver and the kidney. GGSGW is among the most regarded ancient Korean and Chinese herbal formula for insufficiency of kidney qi (the physical substrata and dynamic force of the functional activities of the kidney) [10], edema, frequent urination and weakness and soreness of the loins and the knees. Published and unpublished human clinical studies have supported GGSGW is exerting a certain therapeutic effect on kidney qi deficiency [11]. The safety of the herbs has been acknowledged during their long-standing history of use. In addition, the GV 4 acupoint is selected because it is one of the most effective acupoints for kidney qi deficiency in the traditional theory [12].
Many herbal medicines are injected at acupoints or at disease-related points to treat various symptoms [13]. GGSGW Pharmacopuncture is a new kind of acupuncture treatment based on GGSGW and acupuncture therapy. To our knowledge, no research and no report mentioning the blood pressure and the renal effects of GGSGW Pharmacopuncture have yet been published. The present results provide further insights into the hypotensive and renal effects of GGSGW Pharmacopuncture on global renal function in SHR. Further studies are needed to measure the plasma levels of angiotensin-converting enzyme (ACE) activity and angiotensin II levels in rats during the peak hypotensive response.
The results of this study suggest that the GGSGW Pharmacopuncture has anti-hypertensive effects and improves renal function in SHR. These effects may be related to a decrease in aldosterone caused by treatment with GGSGW Pharmacopuncture. However, the precise mechanism by which GGSGW Pharmacopuncture affect blood pressure in the present experiment remains unknown. Further functional and phytochemical studies are required to establish the effects of GGSGW Pharmacopuncture on the blood pressure and the renal function.