Osteoarthritis (OA) is a chronic degenerative joint disease characterized by damage of articular cartilage and concomitant changes to other articular structures, such as bones, synovium, ligaments, menisci, joint capsules, bursae, and peri-articular muscles (Altman, 2009). It is the most prevalent chronic rheumatic disease that affects women more frequently than men in the aging group and also a major cause of pain and disability in most countries around the globe (Fransen et al., 2011). Most of this disability is attributable to the hips and knees that impairs quality of life, giving significant impact on healthcare costs, employer costs and job performance, and eventually causes enormous economic burden.
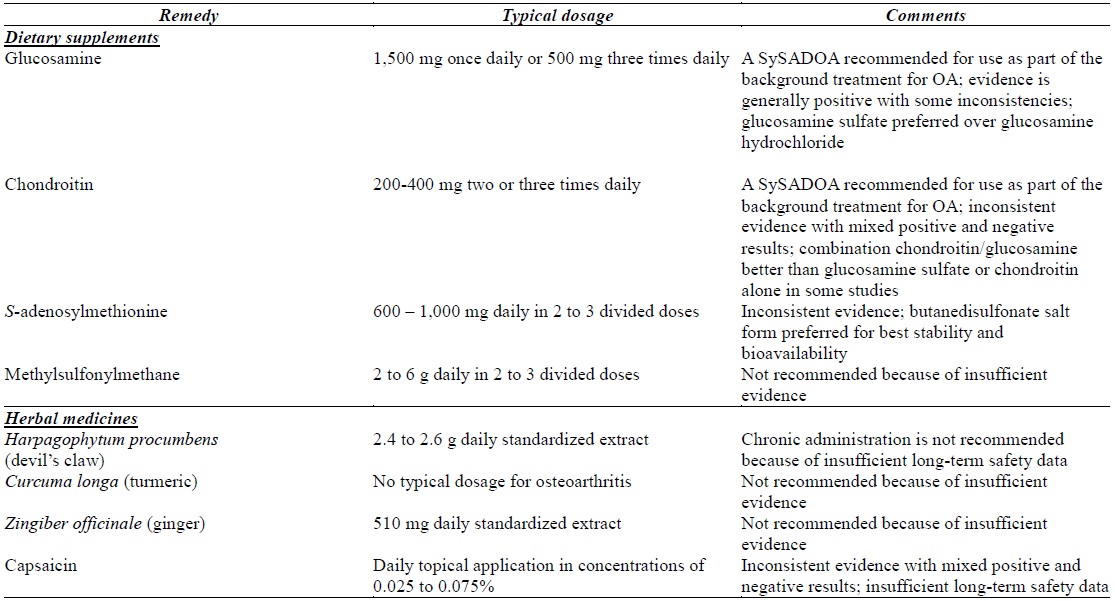
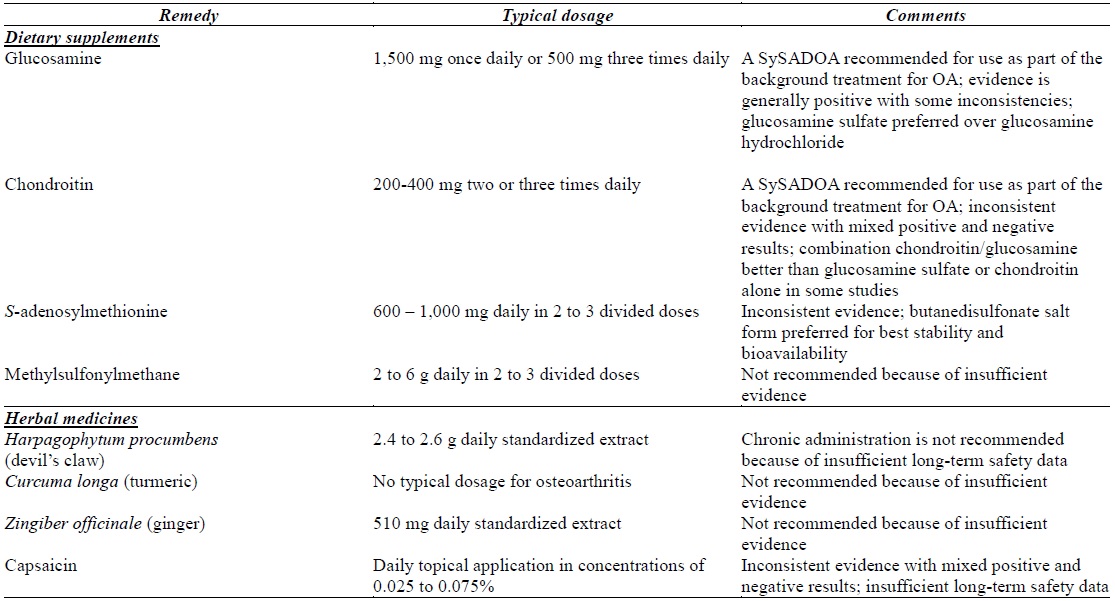
The current medical treatments for osteoarthritis using analgesics and non-steroidal anti-inflammatory drugs (NSAIDs) are focused on relieving pains and symptoms but none are proven to potentially delay the disease progression (Rainsford, 1999). Moreover, NSAIDs are often associated with serious adverse effects in long-term use, such as gastric ulceration, hepatic toxicity, and haemorrhage (Rainsford, 1999; Wolfe et al., 1999). Furthermore, the role of NSAIDs on OA progression remains controversial. Some NSAIDs such as indomethacin are associated with negative effects on chondrocytes and cartilage-matrix formation (Owens et al., 2004) while others (such as nimesulide and naproxen) have chondroprotective effects via increase synthesis of the matrix component (Cheleschi et al., 2015; Notoya et al., 2000). Due to the concern for side effects of NSAIDs and its uncertainty on the cartilage function, patients have opted for safer alternatives that are symptom-modifying and structure-modifying, including herbs, dietary supplements, and non-pharmacological modalities such as physical therapy, acupuncture, exercise and electromagnets (Morelli et al., 2003). Numerous dietary/herbal supplements or formulations targeting patients with OA have been introduced into the market, such as glucosamine, chondroitin, S-adenosylmethionine, methylsulfonylmethane, devil’s claw, turmeric, ginger and capsaicin, but not all of them are proven for long-term safety and effectiveness (Gregory et al., 2008). This review summarizes the efficacy and safety of these remedies which will be discussed in two broad categories: dietary supplements and herbal medicines. Table 1 enlists these natural remedies for OA which will be discussed in the following sections of this review.
[Table 1.] Natural remedies for osteoarthritis
Natural remedies for osteoarthritis
DIETARY SUPPLEMENTS FOR OSTEOARTHRITIS
Glucosamine (2-amino-2-deoxy-ᴅ-glucose) is an amino sugar biosynthesized endogenously in animals and human, with a molecular mass of 179.17 Da. It is water-soluble, with pKa of 7.52 at 20℃ and 6.91 at 37℃ (Setnikar and Rovati, 2001). It is necessary for the generation of glycoprotein and glycosaminoglycans, notably found in synovial fluid, ligaments and other joint structures. These glycosaminoglycans are repeating disaccharide units which are linked together in long chains to a core protein to form the proteoglycan molecule. These proteoglycan molecules are further linked together on one hyaluronic acid filament forming large aggregate proteoglycan macromolecule, of which its moiety gives hyaline cartilage a viscous, elastic resiliency and allows it to act as a cushion. Hyaline cartilage is highly specialized connective tissue comprising chondrocytes and matrix made of collagen and proteoglycan molecules. Therefore the maintenance of articular cartilage and joint architecture depends on the balance between degradation and synthesis of these matrix components.
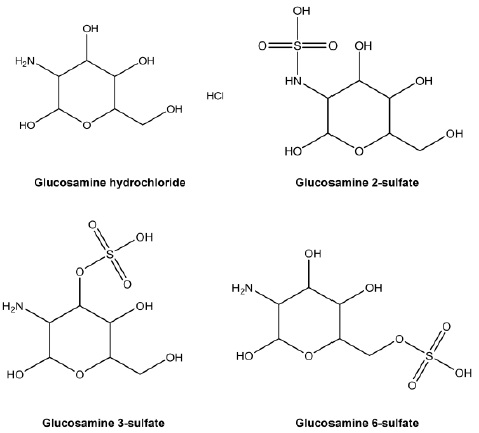
The use of glucosamine in treating arthritic pain can be dated as far back as 1960s (Vetter, 1969) and now it is the most commonly used remedy among osteoarthritic patients. In fact, the current clinical guidelines on OA treatment have recommended the use of glucosamine, and/or chondroitin, as the first line background treatment in conjunction with parallel non-pharmacological therapies (such as weight loss, exercise program, joint braces, insoles, walking aids and acupuncture) in OA patients (Bruyere et al., 2014). Both supplements are currently classified as Symptomatic Slow-Acting Drugs for Osteoarthritis (SySADOAs) in the therapeutic guidelines and are used together with as needed paracetamol for symptomatic relief in patients. Glucosamine is available in multiple forms as over-the-counter supplement, normally in stabilized salt form due to the presence of positively charged amino group of glucosamine at physiological pH that are able to form different conjugates or salts. The widely used forms are glucosamine hydrochloride and glucosamine sulfate (Fig. 1). Exogenous glucosamine is derived from chitin, a polymer present in marine exoskeletons, such as shell fish, or produced synthetically. These exogenous glucosamine may exhibit anti-inflammatory effects and offer a delayed but progressive and longer lasting effect compare to NSAIDs (Bruyere, 2004; Rovati et al., 1999). Moreover, exogenous glucosamine serves mainly as substrate for synthesis of polymers and glycosaminoglycans of joint and bones (Setnikar and Rovati, 2001) and thus, contributes to restoration of damaged cartilage (Bruyere, 2004). Recent in vitro studies have demonstrated that glucosamine acted as a scavenger of free oxygen radicals and was able to control the expression of inflammatory genes and proteins in human chondrocytes (Calamia et al., 2010; Largo et al., 2003). Many proinflammatory factors were found to be reduced by glucosamine including interleukin-1β (IL-1β), tumour necrosis factor (TNF)-α, metalloproteases, prostaglandin (PG) E, as well as superoxide dismutase 2 (Calamia et al., 2010; Largo et al., 2003). A recent Cochrane Review (by the Cochrane Collaboration) has highlighted high-quality trials of the patented glucosamine formulation (crystalline glucosamine sulfate) which showed the superiority of the formulation to placebo in the treatment of pain and functional impairment (Towheed et al., 2009). These trials were long-term studies of 3 months to 3 years duration in OA patients of mild to moderate severity and the results have demonstrated improvement in disease symptoms, joint function and structural changes in patients (Herrero-Beaumont et al., 2007; Pavelka et al., 2002; Reginster et al., 2001).
Glucosamine is usually taken orally at 1,500 mg once daily or 500 mg three times daily, in sulfate or the hydrochloride salt form, or in combination with chondroitin sulfate and methylsulfonylmethane. In terms of pharmacokinetics, the salts of glucosamine are ionized in the stomach, making it available for absorption in the small intestine (Houpt et al., 1999). In humans, 90% of orally administered glucosamine is absorbed from the small intestine. After metabolism in liver, the metabolites of glucosamine are excreted mainly in urine along with the unchanged glucosamine, with a small amount eliminated in the faeces (Setnikar and Rovati, 2001). Due to the first pass metabolism, the bioavailability of orally administered glucosamine is only 25% compared with intravenous administration, which achieves bioactivity of 96% (Barclay et al., 1998). The entry of glucosamine into cells is dependent on stimulation by insulin with the aid of the glucose-transporter system (Pouwels et al., 2001). Healthy humans produce serum glucosamine concentration of around 0.04 mM and would achieve serum level of approximately 0.06 mM after oral intake of glucosamine (Anderson et al., 2005; Pouwels et al., 2001). Acute toxicity studies in animals indicated that very high doses (5,000 – 15,000 mg/kg) of orally administered glucosamine were well tolerated without reports of toxicity, showing a median LD50 value at 8,000 mg/kg (Anderson et al., 2005). Besides, glucosamine is unlikely to cause mutagenicity (Kopsidas and MacPhee, 1994).
On the measure of safety, no significant changes in blood pressure, pulse rate, and other adverse effects were reported for human volunteers who had been infused intravenously with large amount of glucosamine (Pouwels et al., 2001). Most clinical research has reported no pharmacological effects of glucosamine, indicating no interaction of this compound with organs and systems other than joint (Herrero-Beaumont et al., 2007; Reginster et al., 2001). Glucosamine is found to have similar or slightly higher efficacy as compared to NSAIDs treatment on knee OA but that glucosamine exhibited less toxicity (Bruyere, 2004; Houpt et al., 1999). Therefore, it is considered as a safe therapeutic approach to treat OA.
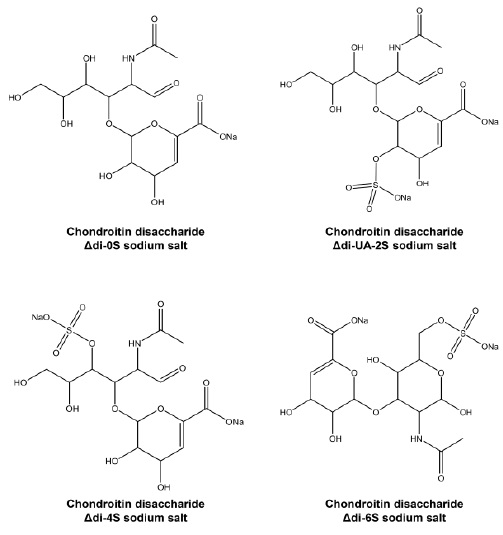
Chondroitin is a negatively charged high molecular weight (10 – 50 kDa) glycosaminoglycan available abundantly in connective tissue and cartilage. It is a natural polymer of a disaccharide comprising repeating sequence of ᴅ-glucuronate and sulphated
Chondroitin as a supplement is produced from animal sources, including shark cartilage and bovine trachea. This supplement, normally in the form of chondroitin sulfate, is orally administered in two or three daily doses of 400 mg (Jackson et al., 2010). The commercially available chondroitin sulfate is normally marketed as co-ingredient with glucosamine. Chondroitin is larger in molecular size and not as well absorbed as glucosamine (Deal and Moskowitz, 1999). It goes through partial digestion in the gastrointestinal tract and an extensive first pass effect, as occurs with other glycosaminoglycans, producing high molecular weight forms or oligosaccharides (Ronca and Conte, 1993). Further breakdown of these products produces mainly the unsaturated disaccharides derived from the chondroitin sulfate molecule itself, including 2-acetamido-2-deoxy-3-O-(β-D-gluco-4-enepyranosyluronicacid)-D-galactose [Δdi-0S], 2-acetamido-2-deoxy-3-O-(β-D-gluco-4-enepyranos-yluronicacid)-2-O-sulfo-D-galactose [Δdi-UA-2S], 2-acet-amido-2-deoxy-3-O-(β-D-gluco-4-enepyranosyluronicacid)-4-O-sulfo-D-galactose [Δdi-4S] and 2-acetamido-2-deoxy-3-O-(β-D-gluco-4-enepyranosyluronicacid)-6-O-sulfo-d-galactose [Δdi-6S]. The chemical structures of these derivatives stabilized in the form of sodium salt are depicted in Fig. 2. These disaccharides are typically detectable in human blood circulation following administration, with high concentration of both Δdi-0S and Δdi-4S and only trace amounts of Δdi-6S and Δdi-UA-2S (Jackson et al., 2010; Okazaki et al., 1995).
Chondroitin sulfate is absorbed to small extent in the small intestine (< 10%), while in the distal gastrointestinal tract, it serves as a prebiotic and is digested further by the enzymes in the intestinal flora to smaller molecules (Barthe et al., 2004). Bioavailability of chondroitin has been estimated at 12 – 13% (Lamari et al., 2006). The elimination half-life of oral administered chondroitin sulfate in human was found to be approximately 5 to 6 hours. About 37 to 50% of the administered chondroitin sulfate is excreted in the urine during the first 24 hour in the forms of high and low molecular weight derivatives (Ronca and Conte, 1993).
As with the case of glucosamine, chondroitin is a SySADOA recommended for use as part of the background treatment for OA (Bruyere et al., 2014). Many clinical studies have confirmed the effectiveness of chondroitin in reducing pain and improving joint mobility in the knee of OA patients (Bucsi and Poór, 1998; Kahan et al., 2009; Mazières et al., 2007; Uebelhart et al., 2004) as well as lowering the number of joints involved in osteoarthritis erosions (Rovetta et al., 2002). These studies were medium- to long-term studies of 6 months to 2 years treatment in OA patients and the results have demonstrated improvement in pain control, joint function and significant reduction in the rate of joint space narrowing. Data from these studies hence have provided evidence for the long-term combined structure modifying and symptom-modifying effects of chondroitin. The therapeutic effects of chondroitin above have been demonstrated to be related to its in vitro activities. In human articular chondrocyte or cartilage cultures, chondroitin was able to increase the production of proteoglycans by inhibition of leukocyte elastase, a serine proteinase which degrades proteoglycans and matrix components (Bassleer et al., 1998). Chondroitin also counteracted IL-1β-induced cartilage damage, including inhibition of activity of chondrocytic metalloproteases and PGE2 release, as well as nitric oxide (NO)-induced apoptosis (Bassleer et al., 1998; Monfort et al., 2005).
The use of glucosamine and chondroitin is believed to bridge symptomatic and preventive approach since these compounds may have the ability to maintain and rebuilt cartilage, with beneficial consequences on both chronic joint pain and progression of joint degeneration. In vivo study and clinical data further indicate that combined use of glucosamine and chondroitin sulfate may have synergistic effect (Fransen et al., 2015; Lippiello et al., 2000), but this effect is somehow inconclusive (Jackson et al., 2010).
S-adenosylmethionine (SAM) is a supplement to treat OA, and also other conditions such as liver disease and depression. It appears to improve chondrocytes and cartilage thickness and may also reduce cytokine-mediated cartilage destruction (Barcelo et al., 1987). Research on the use of SAM for OA however has not been consistent. While some studies have shown its effectiveness in reducing osteoarthritic pain (Maccagno et al., 1987; Najm et al., 2004), SAM can take several weeks of treatment before symptoms improve. Furthermore, as a supplement that requires daily intake, SAM can be expensive (a monthly supply normally costs USD 60-120). Product quality is another concern as SAM is inherently an unstable compound which tends to lose its activity upon storage on the shelves. Hence, SAM may not be a reliable treatment option.
Methylsulfonylmethane (MSM) is typically formulated in combination with glucosamine and/or chondroitin in commercially available supplements. It is promoted as possessing analgesic and anti-inflammatory effects. Preliminary studies in animal models suggest that it may decrease degenerative processes in joints (Ezaki et al., 2013). Clinical trials however yield inconsistent results with modest degree of pain reduction but no effect on joint stiffness (Kim et al., 2006; Usha and Naidu, 2004). In addition, most clinical trials conducted on MSM have been short term and convincing evidence of its long-term efficacy and safety is rather limited, MSM should therefore not be recommended for OA.
HERBAL MEDICINES FOR OSTEOARTHRITIS
>
Harpagophytum procumbens (Devil’s claw)
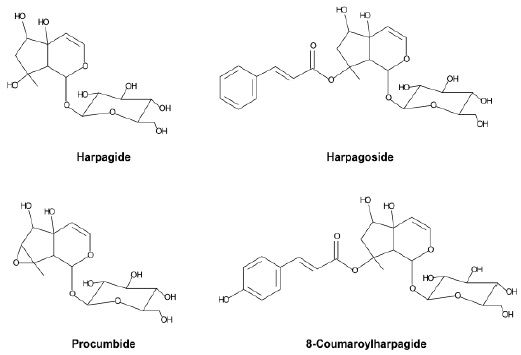
A number of studies have been carried out to prove in vitro and in vivo anti-inflammatory activity for
The effectiveness of
>
Zingiber officinale (Ginger)
Capsaicin is an alkaloid of chili peppers obtained from the plants of genus Capsicum, the most heavily consumed chili throughout the world. Capsaicin and related compounds form a naturally occurring compound group called capsaicinoids, and are responsible for the characteristic pungent flavour and spiciness of chilies. Pharmacological research on capsaicin led to identification of the transient receptor potential channel vanilloid 1 receptor (TRPV1), which is mainly found in sensory neurons (Caterina et al., 1997). Capsaicin is a highly selective and potent agonist of TRPV1 and reduces its heat activation threshold (Knotkova et al., 2008). TRPV1 is a nonselective cation channel with high preference for Ca2+ and is mainly located in nociceptive neurons. It is activated by chemical and physical stimuli, ranging from mechanical pressure to endo/exogenous pain and inflammatory mediators such as heat, low pH, and capsaicin (O’Neill et al., 2012). Prolonged activation of TRPV1 by capsaicin is associated with pain desensitization. Capsaicin-activated TRPV1 goes into a long refractory state and thus a previously excited neuron is resistant to various stimuli (Szallasi and Blumberg, 1999). This process known as defunctionalisation of nociceptive fibres has been exploited for therapeutic use of capsaicin in various painful conditions. Some studies also found an anti-inflammatory potential of capsaicin: it can inhibit paw inflammation in arthritic rats (Joe et al., 1997) and inflammation induced by ethanol at the gastric mucosa in rats (Park et al., 2000). Moreover, capsaicin was reported to inhibit iNOS and COX-2 activity, as well as the NF-kB pathway in macrophages independent from TRPV1 pathway (Kim et al., 2003).
Capsaicin has traditionally been used as a topical rubefacient and counterirritant to relieve pain of muscles and joints. When capsaicin is used for arthritic pain it is typically used as topical preparations, in concentrations of 0.025 or 0.075%, and sold in many countries as lotions, creams and patches intended for daily skin application. Capsaicin was evaluated in a recent systematic review by the Cochrane Collaboration: topical capsaicin was reported not to be effective against osteoarthritis (Cameron and Chrubasik 2013). On the contrary, one meta-analysis found enough evidence to conclude that capsaicin is effective in OA management, although there is a paucity of randomization and adequate blinding in these trials raised by the authors (de Silva et al., 2011). This is in agreement with a further meta-analysis reporting that capsaicin alleviates osteoarthritic pain (Cameron et al., 2009) and another systematic review of recent trials indicating that capsaicin is effective in reducing pain intensity in older adults with painful OA, conferring a medium sized effect (Laslett and Jones, 2014). Nonetheless, despite the promising reports above on its therapeutic use, there remains some uncertainty on whether the capsaicin effect is dose dependent, is consistent across joints, or changes over time. The current literature, at large, lacks multicenter, double blinded, randomised and vehicle-controlled studies in humans, which can ascertain the safety and efficacy of capsaicin.
In this short review, attempts have been made to discuss some commonly used natural remedies for OA treatment. Focus of the discussion has been on the recent evidences of pharmacology, clinical efficacy and safety (whether positive or negative) of these remedies. The aspects discussed are not exhaustive, and they only serve to give a brief overview of the pertinent literature in the field. Furthermore, this is not an all-inclusive comprehensive review of known or potential remedies. Hence the presentation is limited that those remedies where sufficient studies and/or reviews have been reported. Readers can reference some recent articles cited within the text for further information on other remedies. Lastly, scope of this review is only confined to natural remedies, both dietary supplements and herbal medicines, and not non-pharmacological modalities currently used for OA (such as thermal agents, manual therapy, acupuncture, and exercise programs), hence readers should refer to other relevant references for detailed review of this.
Investigations of the in vitro biological activities of glucosamine, chondroitin, S-adenosylmethionine, methylsulfonylmethane,
The authors have no conflicting financial interests.